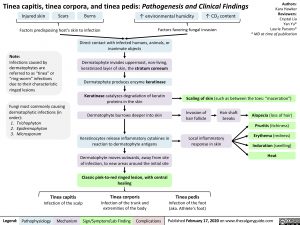
Tinea capitis, tinea corpora, and tinea pedis: Pathogenesis and Clinical Findings
Authors: Kara Hawker Reviewers: Crystal Liu Yan Yu* Laurie Parsons* * MD at time of publication
Injured skin
Scars
Burns
↑ CO2 content Factors favoring fungal invasion
Factors predisposing host’s skin to infection
↑ environmental humidity
Note:
Infections caused by dermatophytes are referred to as “tinea” or “ring-worm” infections due to their characteristic ringed lesions
Fungi most commonly causing dermatophytic infections (in order):
1. Trichophyton
2. Epidermophyton 3. Microsporum
Direct contact with infected humans, animals, or inanimate objects
Dermatophyte invades uppermost, non-living, keratinized layer of skin, the stratum corneum
Dermatophyte produces enzyme keratinase Keratinase catalyzes degradation of keratin
proteins in the skin Dermatophyte burrows deeper into skin
Keratinocytes release inflammatory cytokines in reaction to dermatophyte antigens
Dermatophyte moves outwards, away from site of infection, to new areas around the initial site
Classic pink-to-red ringed lesion, with central healing
Tinea corporis
Scaling of skin (such as between the toes: “maceration”)
Invasion of hair follicle
Hair shaft breaks
Alopecia (loss of hair) Pruritis(itchiness) Erythema (redness) Induration (swelling) Heat
Local inflammatory response in skin
Tinea capitis
Tinea pedis
Infection of the foot (aka. Athlete’s foot)
Infection of the scalp Infection of the trunk and extremities of the body
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published February 17, 2020 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Dermatology Reactive Skin Rash Tinea capitis, tinea corpora, and tinea pedis tinea-capitis-tinea-corpora-and-tinea-pedis