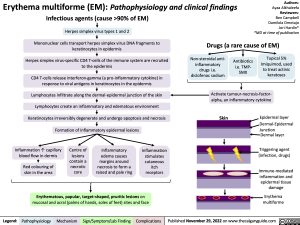
Erythema multiforme (EM): Pathophysiology and clinical findings Infectious agents (cause >90% of EM)
Herpes simplex virus types 1 and 2
Mononuclear cells transport herpes simplex virus DNA fragments to keratinocytes in epidermis
Herpes simplex virus-specific CD4 T-cells of the immune system are recruited to the epidermis
CD4 T-cells release interferon-gamma (a pro-inflammatory cytokine) in response to viral antigens in keratinocytes in the epidermis
Lymphocytes infiltrate along the dermal-epidermal junction of the skin Lymphocytes create an inflammatory and edematous environment Keratinocytes irreversibly degenerate and undergo apoptosis and necrosis Formation of inflammatory epidermal lesions
Authors: Ayaa Alkhaleefa Reviewers: Ben Campbell Damilola Omotajo Jori Hardin* *MD at time of publication
Drugs (a rare cause of EM)
Non-steroidal anti- inflammatory drugs i.e. diclofenac sodium
Antibiotics i.e. TMP- SMX
Topical 5% Imiquimod, used to treat actinic keratoses
Activate tumour-necrosis-factor- alpha, an inflammatory cytokine
Skin
Epidermal layer
Dermal-Epidermal
Junction Dermal layer
Triggering agent (infection, drugs)
Immune-mediated inflammation and epidermal tissue damage
Erythema multiforme
Inflammation ↑ capillary blood flow in dermis
Red colouring of skin in the area
Centre of lesions
contain a necrotic core
Inflammatory edema causes margins around necrosis to form a raised and pale ring
Inflammation stimulates cutaneous itch receptors
Erythematous, papular, target-shaped, pruritic lesions on mucosal and acral (palms of hands, soles of feet) sites and face
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published November 29, 2022 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Dermatology Reactive Skin Rash Erythema multiforme (EM): Pathophysiology and clinical findings Erythema multiforme (EM): Pathophysiology and clinical findings