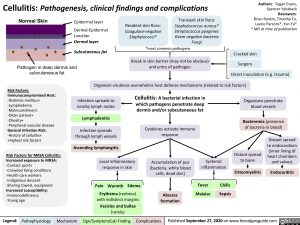
Cellulitis: Pathogenesis, clinical findings and complications
Authors: Tegan Evans, Spencer Yakaback Reviewers: Brian Rankin, Timothy Fu, Laurie Parsons*, Yan Yu* * MD at time of publication
Cracked skin Surgery
Normal Skin
Epidermal layer
Dermal-Epidermal Junction
Dermal layer
Subcutaneous fat
Resident skin flora:
Coagulase-negative Staphylococci*
Transient skin flora:
Staphylococcus aureus* Streptococcus pyogenes Gram negative bacteria Fungi
Pathogen in deep dermis and subcutaneous fat
*most common pathogens
Break in skin barrier (may not be obvious) and entry of pathogen
Risk Factors: Immunocompromised Host: -Diabetes mellitus+ -Lymphedema -Malnourishment
-Older patient+
-Obesity+
-Peripheral vascular disease General Infection Risk: -History of cellulitis+ +highest risk factors
Risk Factors for MRSA Cellulitis: Increased exposure to MRSA: -Contact sports
-Crowded living conditions -Health care workers -Indigenous descent
-Sharing towels, equipment
Increased susceptibility:
-Immunodeficiency -Young age
Direct inoculation (e.g. trauma) Organism virulence overwhelms host defense mechanisms (related to risk factors)
Cellulitis: A bacterial infection in which pathogens penetrate deep dermis and/or subcutaneous fat
Cytokines activate immune response
Accumulation of pus (bacteria, white blood cells, dead skin)
Abscess formation
Infection spreads to nearby lymph nodes
Lymphadenitis
Infection spreads through lymph vessels
Ascending lymphangitis
Local inflammatory response in skin
Pain Warmth Edema Erythema (redness)
with indistinct margins
Vesicles and bullae
Organisms penetrate blood vessels
Bacteremia (presence of bacteria in blood)
Systemic inflammation
Distant spread to bone
Osteomyelitis
Distant spread to endocardium (inner lining of heart chambers and valves)
Endocarditis
Fever Malaise
Chills
Sepsis
(rarely)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published September 27, 2020 on www.thecalgaryguide.com