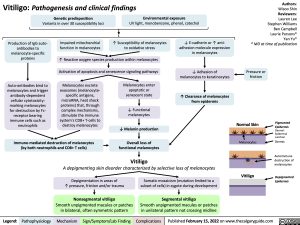
Vitiligo: Pathogenesis and clinical findings
Authors: Wisoo Shin Reviewers: Lauren Lee
Stephen Williams Ben Campbell Laurie Parsons* Yan Yu* * MD at time of publication
Genetic predisposition
Variants in over 30 susceptibility loci
Environmental exposure
UV light, monobenzone, phenol, catechol
Production of IgG auto- antibodies to melanocyte-specific proteins
Auto-antibodies bind to melanocytes and trigger antibody-dependent cellular cytotoxicity: marking melanocytes for destruction by Fc- receptor bearing immune cells such as neutrophils
Impaired mitochondrial function in melanocytes
↑ Susceptibility of melanocytes to oxidative stress
↓ E-cadherin or ↑ anti- adhesion molecule expression in melanocytes
↓ Adhesion of melanocytes to keratinocytes
↑ Clearance of melanocytes from epidermis
↑ Reactive oxygen species production within melanocytes Activation of apoptosis and senescence signaling pathways
Pressure or friction
Melanocytes excrete exosomes (melanocyte- specific antigens, microRNA, heat shock proteins) that, through complex mechanisms, stimulate the immune system’s CD8+ T-cells to destroy melanocytes
Melanocytes enter apoptotic or senescent state
↓ Functional melanocytes
↓ Melanin production
Overall loss of functional melanocytes
Vitiligo
Normal Skin
Pigmented Epidermis Dermal- Epidermal Junction
Dermis
Autoimmune destruction of melanocytes
Depigmented Epidermis
Melanocytes
Immune-mediated destruction of melanocytes (by both neutrophils and CD8+ T cells)
A depigmenting skin disorder characterized by selective loss of melanocytes
Depigmentation in areas of
↑ pressure, friction and/or trauma
Nonsegmental vitiligo
Smooth unpigmented macules or patches in bilateral, often symmetric pattern
Somatic mosaicism (mutation limited to a subset of cells) in zygote during development
Segmental vitiligo
Smooth unpigmented macules or patches in unilateral pattern not crossing midline
Vitiligo
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published February 15, 2022 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Dermatology Other skin lesions Vitiligo: Pathogenesis and Clinical Findings Vitiligo Pathogenesis and Clinical Findings