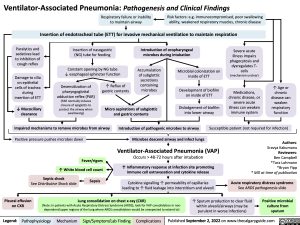
Ventilator-Associated Pneumonia: Pathogenesis and Clinical Findings
Respiratory failure or inability Risk factors: e.g. immunocompromised, poor swallowing
to maintain airway ability, weakened respiratory muscles, chronic disease Insertion of endotracheal tube (ETT) for invasive mechanical ventilation to maintain respiration
Paralytics and
sedatives lead to inhibition of cough reflex
Damage to cilia on epithelial cells of trachea during insertion of ETT
↓ Mucociliary clearance
Insertion of nasogastric (NG) tube for feeding
Constant opening by NG tube ↓ esophageal sphincter function
Introduction of oropharyngeal microbes during intubation
Severe acute illness impairs phagocytosis and dysregulates T- cells (mechanism unclear)
Medications, chronic disease, or severe acute illness can weaken immune system
Desensitization of
pharyngoglottal
adduction reflex (PAR) (PAR normally induces closure of epiglottis to protect the airway when swallowing)
↑ Reflux of gastric contents
Accumulation of subglottic secretions containing microbes
Microbial colonization on inside of ETT
Development of biofilm on inside of ETT
Dislodgement of biofilm into lower airway
↑ Age or chronic disease can weaken respiratory function
Micro aspirations of subglottic and gastric contents
Impaired mechanisms to remove microbes from airway Positive pressure pushes microbes down
Fever/rigors ↑ White blood cell count
Introduction of pathogenic microbes to airway Susceptible patient (not required for infection)
Septic shock
See Distributive Shock slide
Sepsis
Microbes descend airway and infect lungs
Ventilator-Associated Pneumonia (VAP)
Occurs > 48-72 hours after intubation
↑ Inflammatory response at infection site promoting immune cell extravasation and cytokine release
Cytokine signalling ↑ permeability of capillaries leading to ↑ fluid leakage into interstitium and alveoli
Authors: Sravya Kakumanu Reviewers: Ben Campbell *Tara Lohmann *Bryan Yipp * MD at time of publication
Acute respiratory distress syndrome
See ARDS pathogenesis slide
Pleural effusion Lung consolidation on chest x-ray (CXR) ↑ Sputum production to clear fluid on CXR (Note: In patients with Acute Respiratory Distress Syndrome (ARDS), look for VAP consolidation in non- within alveoli/airways (may be
Positive microbial culture from sputum
dependent/upper regions of the lung where ARDS consolidation would be unexpected to extend to)
purulent in worse infections)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published September 2, 2022 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Respirology Respiratory Infections Ventilator-Associated Pneumonia: Pathogenesis and Clinical Findings ventilator-associated-pneumonia-pathogenesis-and-clinical-findings