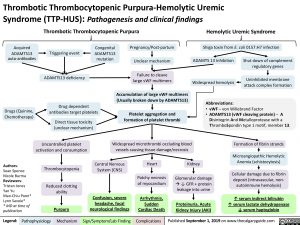
Thrombotic Thrombocytopenic Purpura-Hemolytic Uremic Syndrome (TTP-HUS): Pathogenesis and clinical findings
Thrombotic Thrombocytopenic Purpura
Hemolytic Uremic Syndrome
Shiga toxin from E. coli 0157:H7 infection
Acquired
ADAMTS13 auto-antibodies
Pregnancy/Post-partum Unclear mechanism
Failure to cleave large vWF multimers
Accumulation of large vWF multimers (Usually broken down by ADAMTS13)
Platelet aggregation and formation of platelet thrombi
Widespread microthrombi occluding blood vessels causing tissue damage/necrosis
Congenital ADAMTS13 mutation
Triggering event
ADAMTS13 deficiency
Drug dependent antibodies target platelets
Direct tissue toxicity (unclear mechanism)
ADAMTS 13 Inhibition Widespread hemolysis
Shut down of complement regulatory genes
Uninhibited membrane attack complex formation
Drugs (Quinine, Chemotherapy)
Abbreviations:
• vWF – von Willebrand Factor
• ADAMTS13 (vWF cleaving protein) – A
Disintegrin And Metalloprotease with a ThromboSpondin type 1 motif, member 13.
Formation of fibrin strands
Microangiopathic Hemolytic Anemia (schistocytosis)
Cellular damage due to fibrin deposit (intravascular, non- autoimmune hemolysis)
↑ serum indirect bilirubin
↑ serum lactate dehydrogenase ↓ serum haptoglobin
Authors:
Sean Spence Nicole Burma Reviewers: Tristan Jones Yan Yu Man-Chiu Poon* Lynn Savoie*
* MD at time of publication
Uncontrolled platelet activation and consumption
Thrombocytopenia
Reduced clotting ability
Purpura
Central Nervous System (CNS)
Confusion, severe headache, focal neurological findings
Heart
Patchy necrosis of myocardium
Arrhythmia, Sudden Cardiac Death
Kidney
Glomerular damage à↓ GFR + protein leakage into urine
Proteinuria, Acute Kidney Injury (AKI)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published September 1, 2019 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Hematology Blood Clotting Disorders Thrombotic Thrombocytopenic Purpura-Hemolytic Uremic Syndrome (TTP-HUS): Pathogenesis and clinical findings Thrombotic Thrombocytopenic Purpura-Hemolytic Uremic Syndrome (TTP-HUS): Pathogenesis and clinical findings