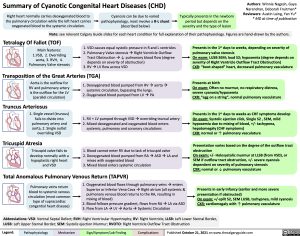
Summary of Cyanotic Congenital Heart Diseases (CHD)
Authors: Winnie Nagesh, Gaya Narendran, Deborah Fruitman* Reviewers: Austin Laing, Yan Yu* * MD at time of publication
Right heart normally carries deoxygenated blood to the pulmonary circulation while the left heart carries oxygenated blood to the systemic circulation.
Cyanosis can be due to varied pathophysiology, most involve a R-L shunt (described below)
Typically presents in the newborn period but depends on the severity and the type of lesion
Tetralogy Of Fallot (TOF)
Main features: 1.VSD, 2. Overriding aorta, 3. RVH, 4. Pulmonary Valve stenosis
1. VSD causes equal systolic pressure in R and L ventricles
2. Pulmonary Valve stenosisàRight Ventricle Outflow
Tract Obstructionà↓ pulmonary blood flow (degree
depends on severity of obstruction)
3. RVàLV flow across VSD
Presents in the 1st days to weeks, depending on severity of pulmonary valve stenosis
On exam: LUSB SEM; loud S2; hypoxemia (degree depends on severity of Right Ventricle Outflow Tract Obstruction)
CXR: “boot-shaped” heart, decreased pulmonary vasculature
Presents at birth
On exam: Often no murmur, no respiratory distress, severe cyanosis/hypoxemia
CXR: “egg on a string”, normal pulmonary vasculature
Presents in the 1st days to weeks as CHF symptoms develop On exam: Systolic ejection click, Single S2 , SEM, mild hypoxemia due to mixing of blood, +/- tachypnea, hepatomegaly (CHF symptoms)
CXR: normal or ↑ pulmonary vasculature
Presentation varies based on the degree of the outflow tract obstruction
On exam: +/- Holosystolic murmur at LLSB (from VSD), or SEM if outflow tract obstruction, +/- severe cyanosis dependent on severity of pulmonary stenosis
CXR: normal or ↓ pulmonary vasculature
Presents in early infancy (earlier and more severe presentation if obstructed)
On exam: +/-split S2, SEM LUSB, tachypnea, mild cyanosis CXR: cardiomegaly with ↑ pulmonary vasculature
Note: see relevant Calgary Guide slides for each heart condition for full explanation of their pathophysiology. Figures are hand-drawn by the authors.
Transposition of the Great Arteries (TGA)
Aorta is the outflow for RV and pulmonary artery is the outflow for the LV (parallel circulation)
Truncus Arteriosus
1. Single vessel (truncus) fails to divide into pulmonary artery and aorta, 2. Single outlet overriding VSD
Tricuspid Atresia
Tricuspid valve fails to develop normally with a
hypoplastic right heart and VSD
1. Deoxygenated blood pumped from RVàaortaà systemic circulation, bypassing the lungs.
2. Oxygenated blood pumped from LVàPA
1. RV + LV pumped through VSDàoverriding truncal artery 2. Mixed deoxygenated and oxygenated blood enters
systemic, pulmonary and coronary circulations
1. Blood cannot enter RV due to lack of tricuspid valve
2. Deoxygenated blood pumped from RAàASDàLA and
mixes with oxygenated blood
3. Mixed blood enters systemic circulation
Total Anomalous Pulmonary Venous Return (TAPVR)
Pulmonary veins return blood to systemic venous circulation (most common type of supracardiac congential heart disease)
1. Oxygenated blood flows through pulmonary veinsàenters Superior or Inferior Vena CavaàRight atrium (all systemic & pulmonary venous blood returns to the RA, resulting in mixing of blood)
2. Blood follows pressure gradient, flows from RAàLA via ASD
3. Flow from LAàLVàAortaàSystemic Circulation
Abbreviations: VSD: Ventral Septal Defect; RVH: Right Ventricular Hypertrophy; RV: Right Ventricle, LLSB: Left Lower Sternal Border, LUSB: Left Upper Sternal Border; SEM: Systolic ejection Murmur; RVOTO: Right Ventricle Outflow Tract Obstruction
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published October 21, 2021 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Cardiology Cyanotic Congenital Heart Disease Summary of Cyanotic Congenital Heart Diseases Summary of Cyanotic Congenital Heart Diseases