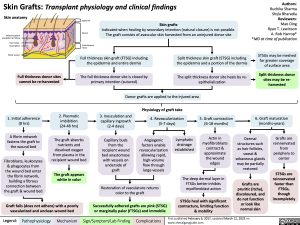
Skin Grafts: Transplant physiology and clinical findings
Authors: Ruchika Sharma Shyla Bharadia Reviewers: Mao Ding Ryan T. Lewinson A. Rob Harrop* *MD at time of publication
STSGs may be meshed for greater coverage of surface area
Split thickness donor sites may be re- harvested
6. Graft maturation (months-years)
Skin anatomy
Sebaceous gland alongside hair follicle
Hair Follicle Sweat gland
Blood vessels
Full thickness donor sites cannot be re-harvested
Epidermis
Dermis
Subcutaneous tissue
Full thickness skin graft (FTSG) including the epidermis and entire dermis
The full thickness donor site is closed by primary intention (sutured)
Skin grafts
Indicated when healing by secondary intention (natural closure) is not possible. The graft consists of avascular skin harvested from an uninjured donor site
Split thickness skin graft (STSG) including the epidermis and a portion of the dermis
The split thickness donor site heals by re- epithelialization
Donor grafts are applied to the injured area
1. Initial adherence (8 hrs)
A fibrin network fastens the graft to the wound bed
Fibroblasts, leukocytes & phagocytes from the wound bed enter the fibrin network, building a fibrous connection between the graft & wound bed
2. Plasmatic imbibition (24-48 hrs)
The graft absorbs nutrients and dissolved oxygen from plasma in the recipient wound bed
The graft appears white in color
3. Inosculation and capillary ingrowth (2-4 days)
Capillary buds from the recipient wound bed anastomose with vessels on underside of graft
Physiology of graft take
4. Revascularization (5-7 days)
5. Graft contraction (6-18 months)
Actin in myofibroblasts contract & approximate the wound edges
Angiogenic factors enable revascularization allowing rapid, high-volume flow through large vessels
Lymphatic drainage established
Dermal structures such as hair follicles, sweat & sebaceous glands may be partially restored
Grafts are pruritic (itchy), discoloured, and do not function or look like normal skin
Grafts are reinnervated from periphery to center
STSGs are reinnervated faster than FTSGs, though incompletely
Graft fails (does not adhere) with a poorly vascularized and unclean wound bed
Restoration of vasculature returns color to the graft
Successfully adhered grafts are pink (STSG) or marginally paler (FTSGs) and immobile
The deep dermal layer in FTSGs better inhibits myofibroblast action
STSGs heal with significant contracture, limiting function & mobility
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
First published February 6, 2017, updated March 12, 2023 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Dermatology Burns Skin Grafts: Transplant Physiology and Clinical Findings Skin Grafts Transplant physiology and clinical findings