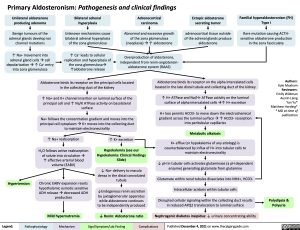
Primary Aldosteronism: Pathogenesis and clinical findings
Unilateral aldosterone producing adenoma
Benign tumours of the adrenal glands develop ion channel mutations
↑ Na+ movement into adrenal gland cellsàcell depolarizationà↑ Ca+ entry into zona glomerulosa
Bilateral adrenal hyperplasia
Unknown mechanisms cause bilateral adrenal hyperplasia of the zona glomerulosa
↑ Ca+ leads to cellular replication and hyperplasia of the zona glomerulosaà ↑aldosterone release
Adrenocortical carcinoma
Abnormal and excessive growth of the zona glomerulosa (neoplasia)à↑ aldosterone
Overproduction of aldosterone, independent from renin-angiotensin- aldosterone system (RAAS)
Ectopic aldosterone secreting tumor
adrenocortical tissue outside of the adrenal glands produce aldosterone
Familial hyperaldosteronism (FH) Type I
Rare mutation causing ACTH- sensitive aldosterone production in the zona fasciculata
Aldosterone binds its receptor on the principal cells located in the collecting duct of the kidney
↑ Na+ and K+ channel insertion on luminal surface of the principal cell and ↑ Na/K ATPase activity on basolateral surface
Na+ follows the concentration gradient and moves into the principal cell cytoplasmàK+ moves into the collecting duct to maintain electroneutrality
Aldosterone binds its receptor on the alpha intercalated cells located in the late distal tubule and collecting duct of the kidney
↑ H+ ATPase and Na/H+ ATPase activity on the luminal surface of alpha intercalated cellsà↑ H+ excretion
H+ loss permits HCO3- to move down the electrochemical gradient across the luminal surfaceà↑ HCO3- resorption into peritubular capillaries
Metabolic alkalosis
K+ efflux (or hypokalemia of any etiology) is counterbalanced by influx of H+ into tubular cells to maintain electroneutrality
↓ pH in tubular cells activates glutaminase (a pH dependent enzyme) generating glutamate from glutamine
Glutamate within renal tubules dissociates into NH4+, HCO3- Intracellular acidosis within tubular cells
Disrupted cellular signaling within the collecting duct results in reduced APQ2 translocation to luminal surface
Authors: Kyle Moxham Reviewers: Emily Wildman Austin Laing Yan Yu* Matthew Harding* * MD at time of publication
Hypertension
↑ Na+ reabsorption
H2O follows active reabsorption
of solute into circulationà ↑ effective arterial blood volume (EABV)
Chronic EABV expansion resets hypothalamic osmotic sensitive ADH releaseàdecreased ADH production
↑ K+ excretion
Hypokalemia (see our Hypokalemia: Clinical Findings Slide)
↓ Na+ delivery to macula densa in the distal convoluted tubule
↓Endogenous renin secretion by juxtaglomerular apparatus while aldosterone continues to be independently produced
Polydipsia & Polyuria
Mild hypernatremia
↓ Renin: Aldosterone ratio
Nephrogenic diabetes insipidus: ↓ urinary concentrating ability
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published December 4, 2021 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Endocrinology Adrenal Disorders Primary Aldosteronism: Pathogenesis and Clinical Findings Primary Aldosteronism Pathogenesis