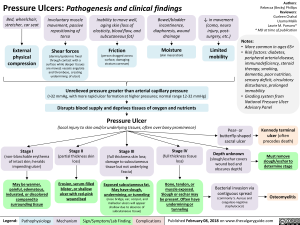
Depth unknown (slough/eschar covers wound bed and obscures depth)
Must remove slough/eschar to determine stage
-110.
Kennedy terminal ulcer (often precedes death)
—1111.
Pressure Ulcers: Pathogenesis and clinical findings
Bed, wheelchair, stretcher, car seat
External physical compression
Involuntary muscle movement, passive repositioning of torso Shear forces (dermis/epidermis fixed through contact with a surface while deeper tissues are moved; vessels angulate and thrombose, creating undermining of ulcer)
Inability to move well, aging skin (loss of elasticity, blood flow, and subcutaneous fat) Friction (person dragged across surface, damaging stratum corneum)
Bowel/bladder incontinence, diaphoresis, wound drainage Moisture (skin maceration)
4, in movement (coma, neuro injury, post-surgery, etc.) Limited mobility
Unrelieved pressure greater than arterial capillary pressure (>32 mmHg, with more rapid ulcer formation at higher pressures; normal range 12-32 mmHg) Disrupts blood supply and deprives tissues of oxygen and nutrients Pressure Ulcer (local injury to skin and/or underlying tissues, often over bony prominence)
Authors: Rebecca (Becky) Phillips Reviewers: Gurleen Chahal Usama Malik Laurie M. Parsons* * MD at time of publication
Notes: • More common in ages 65+ • Risk factors: diabetes, peripheral arterial disease, immunodeficiency, steroid therapy, smoking, dementia, poor nutrition, sensory deficit, circulatory disturbance, prolonged immobility • Grading system from National Pressure Ulcer Advisory Panel
Pear- or butterfly-shaped sacral ulcer
Stage I (non-blanchable erythema of intact skin; heralds impending ulcer)
May be warmer, painful, edematous, indurated, or discolored compared to surrounding tissue
Legend:
Stage II (partial thickness skin loss)
Erosion, serum-filled blister, or shallow ulcer with red-pink wound bed
Pathophysiology Mechanism
Stage III (full thickness skin loss; damage to subcutaneous tissue but not underlying fascia)
*
Exposed subcutaneous fat. May have slough, undermining, or tunneling (nose bridge, ear, occiput, and malleolar ulcers will appear shallow due to absence of subcutaneous tissue)
Sign/Symptom/Lab Finding
Stage IV (full thickness tissue loss)
Bone, tendon, or muscle exposed. Slough or eschar may be present. Often have undermining or tunneling
Complications
Bacterial invasion via contiguous spread (commonly S. Aureus and coagulase-negative staphylococci)
Osteomyelitis