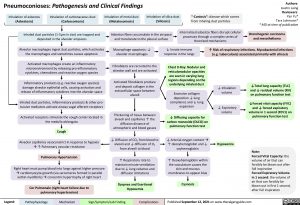
Pneumoconioses: Pathogenesis and Clinical Findings
Authors: Austin Laing
Reviewers: Yan Yu* Tara Lohmann* * MD at time of publication
Bronchogenic carcinoma and mesothelioma
Inhalation of asbestos
(Asbestosis)
Inhalation of carbonaceous dust
(Carboconiosis)
Inhalation of metal dust
(Metaloconiosis)
Inhalation of silica dust
(Silicosis)
“-Coniosis”: disease which comes from inhaling dust particles
Internalized asbestos fibers disrupt cellular processes through a complex series of theorized mechanisms
Inhaled dust particles (1-5μm in size) are trapped and deposited in the alveolar airspaces
Alveolar macrophages ingest dust particles, which activates the macrophages and sometimes causes apoptosis
Activated macrophages create an inflammatory microenvironment by releasing pro-inflammatory cytokines, chemokines and reactive oxygen species
Inflammatory products (e.g. reactive oxygen species) damage alveolar epithelial cells, causing activation and release of inflammatory cytokines into the alveolar space
Inhaled dust particles, inflammatory products & other pro- tussive mediators activate airway vagal afferent receptors
Activated receptors stimulate the cough center located in the medulla oblongata
Cough
Alveolar capillaries vasoconstrict in response to hypoxia à↑ Pulmonary vascular resistance
Pulmonary Hypertension
Right heart must pump blood into lungs against higher pressure àcardiomyocyte growth (via sarcomeres formed in parallel within myofibrils)àconcentric hypertrophy of right heart
Cor Pulmonale (right heart failure due to pulmonary hypertension)
Asbestos fibers accumulate in the airspace and translocate to the pleural surface
Macrophage apoptosis: ↓ alveolar macrophages
Fibroblasts are recruited to the alveolar wall and are activated
Activated fibroblasts produce and deposit collagen in the
extracellular space between alveoli
Thickening of tissue between alveoli and capillaries ↑ the diffusion distance of atmospheric and blood gasses
↓ Diffusion of CO2 from blood to alveoli and ↓ diffusion of O2 from alveoli to blood
↑ Respiratory rate to maintain minute ventilation due to ↓ lung volumes and diffusion limitations
Dyspnea and Exertional Hypoxemia
↓ Innate immune response in the lungs
Chest X-Ray: Nodular and reticulonodular opacities are seen in varying lung regions depending on the underlying inhaled dust
Excessive collagen
deposition ↓ lung compliance and ↓ lung expansion
↓ Diffusing capacity for carbon monoxide (DLCO) on pulmonary function test
↓ Arterial oxygen contentà ↑ deoxyhemoglobin and ↓ oxyhemoglobin
↑ Deoxyhemoglobin within the vasculature causes the skin and mucous membranes to appear blue
Cyanosis
↑ Risk of respiratory infections. Mycobacterial infections (e.g. tuberculosis) associated primarily with silicosis
↓ Inhalation volume
↓ Expiratory volume
Hypoxemia
↓Total lung capacity (TLC) and ↓ residual volume (RV) on pulmonary function test
↓Forced vital capacity (FVC) and ↓ forced expiratory volume in 1 second (FEV1) on pulmonary function test
Note:
Forced Vital Capacity: the volume of air that can forcibly be blown out after full inspiration
Forced Expiratory Volume in 1 second: the volume of air that can forcibly be blown out in first 1 second, after full inspiration
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published September 12, 2021 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Respirology Other Causes of Dyspnea Pneumoconioses: Pathogenesis and Clinical Findings Pneumoconioses