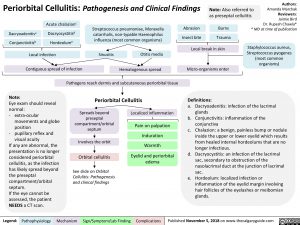
Periorbital Cellulitis: Pathogenesis and Clinical Findings
Authors: Amanda Marchak Reviewers: Jaimie Bird Dr. Rupesh Chawla* * MD at time of publication
Staphylococcus aureus, Streptococcus pyogenes (most common organisms)
Note: Also referred to as preseptal cellulitis
Dacryoadenitisa Conjunctivitisb
Acute chalazionc
Dacryocystitisd Hordeolume
Streptococcus pneumoniae, Moraxella catarrhalis, non-typable Haemophilus influenza (most common organisms)
Abrasion Insect bite
Burns Trauma
Local infection
Contiguous spread of infection
Sinusitis
Otitis media Hematogenous spread
Local break in skin Micro-organisms enter
Definitions:
Note:
Eye exam should reveal normal:
– extra-ocular
movements and globe
position
– pupillary reflex and
visual acuity
If any are abnormal, the presentation is no longer considered periorbital cellulitis, as the infection has likely spread beyond the preseptal compartment/orbital septum.
If the eye cannot be assessed, the patient NEEDS a CT scan.
Pathogens reach dermis and subcutaneous periorbital tissue
Periorbital Cellulitis
a. Dacryoadenitis: infection of the lacrimal glands
b. Conjunctivitis: inflammation of the conjunctiva
c. Chalazion: a benign, painless bump or nodule inside the upper or lower eyelid which results from healed internal hordeolums that are no longer infectious.
d. Dacryocystitis: an infection of the lacrimal sac, secondary to obstruction of the nasolacrimal duct at the junction of lacrimal sac.
e. Hordeolum: localized infection or inflammation of the eyelid margin involving hair follicles of the eyelashes or meibomian glands.
Spreads beyond preseptal compartment/orbital septum
Involves the orbit Orbital cellulitis
See slide on Orbital Cellulitis: Pathogenesis and clinical findings
Localized inflammation
Pain on palpation
Induration
Warmth
Eyelid and periorbital edema
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published November 5, 2018 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Infectious Diseases Pediatric Periorbital Cellulitis: Pathogenesis and Clinical Findings Periorbital Cellulitis: Pathogenesis and Clinical Findings