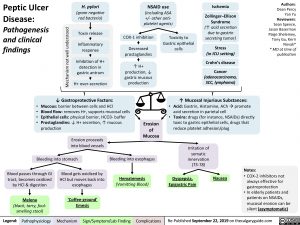
Peptic Ulcer Disease:
Pathogenesis and clinical findings
H. pylori
(gram negative rod bacteria)
Toxin release
Inflammatory response
Inhibition of H+ detection in gastric antrum
H+ over-secretion
NSAID use
(including ASA
+/- other anti- platelet agents)
Ischemia
Zollinger–Ellison Syndrome (↑ acid secretion due to gastrin secreting tumor)
Stress
(in ICU setting)
Crohn’s disease
Cancer
(adenocarcinoma, SCC, lymphoma)
↑ Mucosal Injurious Substances: Acid: Gastrin, Histamine, AChàpromote
acid secretion in parietal cell
Toxins: drugs (for instance, NSAIDs) directly toxic to gastric epithelial cells, drugs that reduce platelet adhesion/plug
Authors: Dean Percy Yan Yu Reviewers: Sean Spence, Jason Baserman Paige Shelemey, Tony Gu, Kerri Novak* * MD at time of publication
COX-1 inhibition
Decreased prostaglandins
↑ H+ production, ↓
gastric mucous production
Toxicity to Gastric epithelial cells
↓ Gastroprotective Factors:
• Mucous: barrier between cells and HCl
• Blood flow: removes H+, supports mucosal cells
• Epithelial cells: physical barrier, HCO3- buffer
• Prostaglandins: ↓ H+ secretion, ↑ mucous
• •
production
Erosion of Mucosa
Erosion proceeds into blood vessels
Irritation of somatic innervation (T5-T8)
Bleeding into stomach
Bleeding into esophagus
Hematemesis
(Vomitting Blood)
Blood passes through GI tract, becomes oxidized by HCl & digestion
Melena
(black, tarry, foul- smelling stool)
Blood gets oxidized by HCl but moves back into esophagus
‘Coffee-ground’ Emesis
Notes:
Dyspepsia, Epigastric Pain
Nausea
• COX-2 inhibitors not always effective for gastroprotection
• In elderly patients and patients on NSAIDs, mucosal erosion can be silent (asymptomatic)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-Published September 22, 2019 on thecalgaryguide.com
Mechanism not well understood