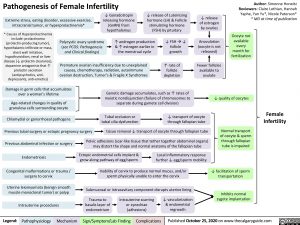
Pathogenesis of Female Infertility
Author: Simonne Horwitz Reviewers: Claire Lothian, Hannah Yaphe, Yan Yu*, Nicole Paterson* * MD at time of publication
Extreme stress, eating disorder, excessive exercise, intracranial tumor, or hyperprolactinemia*
↓ Gonadotropin releasing hormone (GnRN) from hypothalamus
↓ release of Luteinizing hormone (LH) & Follicle stimulating hormone (FSH) by pituitary
↓ release of estrogen by ovaries
Anovulation (oocyte is not released)
Fewer follicles available to ovulate
* Causes of Hyperprolactinemia include: prolactinoma (prolactin-producing tumor), hypothalamic infiltrate or mass, chest wall irritation, hypothyroidism, renal or liver disease (↓ prolactin clearance), dopamine antagonists that ↑ prolactin secretion (antipsychotics, anti- depressants, anti-emetics)
Polycystic ovary syndrome (see PCOS: Pathogenesis and Clinical findings)
↑ androgen production & ↑ estrogen earlier in the menstrual cycle
↓ FSHà↓ follicle growth
↑ rate of follicle depletion
Oocyte not available every month for fertilization
Premature ovarian insufficiency due to unexplained causes, chemotherapy, radiation, autoimmune ovarian destruction, Turner’s & Fragile X Syndromes
Damage in germ cells that accumulates over a woman’s lifetime
Age-related changes in quality of granulosa cells surrounding oocyte
Genetic damage accumulates, such as ↑ rates of meiotic nondisjunction (failure of chromosomes to separate during gamete cell division)
Tubal occlusion or ↓ transport of oocyte tubal cilia dysfunction through fallopian tube
↓ quality of oocytes
Normal transport of oocyte & sperm through fallopian tube is impaired
↓ facilitation of sperm transportation
Inhibits normal zygote implantation
Chlamydial or gonorrhoeal pathogens
Previous tubal surgery or ectopic pregnancy surgery tissue removal ↓ transport of oocyte through fallopian tube
Female Infertility
Previous abdominal infection or surgery Endometriosis
Congenital malformations or trauma / surgery to cervix
Uterine leiomyomata (benign smooth muscle monoclonal tumor) or polyp
Intrauterine procedures
Pelvic adhesions (scar-like tissue that tether together abdominal organs) may distort the shape and normal anatomy of the fallopian tube
Ectopic endometrial cells implant & Local inflammatory response grow along pathway of egg/sperm further ↓ egg/sperm mobility
Inability of cervix to produce normal mucus, and/or sperm physically unable to enter the cervix
Submucosal or intracavitary component disrupts uterine lining
Trauma to basalis layer of endometrium
Intrauterine scarring or synechiae (adhesions)
↓ vascularization & endometrial regrowth
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published October 25, 2020 on www.thecalgaryguide.com