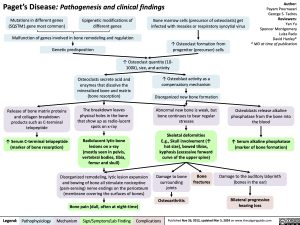
Paget’s Disease: Pathogenesis and clinical findings
Author: Payam Pournazari George S. Tadros Reviewers: Yan Yu Spencer Montgomery Luiza Radu David Hanley* * MD at time of publication
Mutations in different genes (SQSTM1 gene most common)
Epigenetic modifications of different genes
Bone marrow cells (precursor of osteoclasts) get infected with measles or respiratory syncytial virus
↑ Osteoclast formation from progenitor (precursor) cells
Malfunction of genes involved in bone remodeling and regulation
Genetic predisposition
↑ Osteoclast quantity (10- 100X), size, and activity
Release of bone matrix proteins and collagen breakdown products such as C-terminal telopeptide
↑ Serum C-terminal telopeptide (marker of bone resorption)
Osteoclasts secrete acid and enzymes that dissolve the mineralized bone and matrix (bone resorption)
The breakdown leaves physical holes in the bone that show up as radio-lucent spots on x-ray
Radiolucent lytic bone lesions on x-ray (mostly seen in pelvis, vertebral bodies, tibia, femur and skull)
↑ Osteoblast activity as a compensatory mechanism
Disorganized new bone formation
Abnormal new bone is weak, but bone continues to bear regular stresses
Skeletal deformities E.g., Skull involvement (↑ hat size), bowed tibias, kyphosis (excessive forward curve of the upper spine)
Osteoblasts release alkaline phosphatase from the bone into the blood
↑ Serum alkaline phosphatase (marker of bone formation)
Damage to the auditory labyrinth (bones in the ear)
Bilateral progressive hearing loss
Disorganized remodeling, lytic lesion expansion and bowing of bone all stimulate nociceptive (pain-sensing) nerve endings on the periosteum (membrane covering the surfaces of bones)
Bone pain (dull, often at night-time)
Damage to bone surrounding joints
Osteoarthritis
Bone fractures
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published Nov 26, 2012, updated Mar 5, 2024 on www.thecalgaryguide.com
Paget’s Disease: Pathogenesis and clinical findings
Author: Payam Pournazari George S. Tadros Reviewers: Yan Yu Spencer Montgomery David Hanley* * MD at time of publication
Mutations in different genes (SQSTM1 gene most common, but also TNFRSF11A, ZNF687 and PFN1)
Epigenetic modifications of different genes (including RANKL, OPG, HDAC2, DNMT1, and SQSTM1)
Malfunction of genes involved in bone remodeling and regulation
Possible viral exposure (measles or respiratory syncytial virus)
Genetic predisposition
↑ Osteoclast quantity (10- 100X), size, and activity
Release of bone matrix proteins and collagen breakdown products such as C-terminal telopeptide (CTx)
↑ Serum C-terminal telopeptide
marker of bone resorption
Osteoclasts secrete acid and enzymes that dissolve the mineralized bone and matrix (bone resorption)
The breakdown leaves physical holes in the bone
that show up as radio-lucent spots on x-ray
Radiolucent Lytic bone lesions on x-ray (mostly seen in pelvis, vertebral bodies, tibia, femur and skull)
↑ Osteoblast activity as a compensatory mechanism
Disorganized new bone formation
Abnormal new bone is weak, but bone continues to bear regular stresses
Skeletal deformities
E.g., Skull involvement (↑ hat size), Bowed tibias, kyphosis (excessive forward curve of the upper spine)
Osteoblasts release Alkaline Phosphatase (ALP) from the bone into the blood
↑ Serum Alkaline Phosphatase
marker of bone formation
Damage to the auditory labyrinth (bones in the ear)
Bilateral progressive hearing loss
Disorganized remodeling, lytic lesion expansion and bowing of bone all stimulate nociceptive (pain-sensing) nerve endings on the periosteum (membrane covering the surfaces of bones)
Bone pain (dull, often at night-time)
Damage to bone surrounding joints
Osteoarthritis
Bone fractures
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published November 26, 2012 on www.thecalgaryguide.com
Paget’s disease: Pathogenesis, Clinical Findings
Author: Payam Pournazari Reviewers: Yan Yu Spencer Montgomery David Hanley* * MD at time of publication
Genetic predisposition (possibly in RANK encoding gene)
Possible viral exposure (measles and respiratory syncytial virus)
↑ in number (10-100X), size, and activity of osteoclasts
Osteoclasts cause excessive bone resorption, which also stimulates osteoblasts
Release of bone matrix proteins and collagen breakdown products such as C-terminal telopeptide of pyridinoline crosslinks (CTx)
↑ serum CTx
marker of bone resorption
Osteoclasts secrete acid and enzymes that dissolve the mineralized bone and matrix
Leaves physical holes in the bone that show up as radio- lucent spots on x-ray
Lytic bone lesions
(mostly seen in pelvis, vertebral bodies, tibia, femur and skull)
Marked ↑ osteoblastic activity results in disorganized new bone formation
Abnormal new bone bone is weak, but bone continues to bear regular stresses
Skeletal deformities: e.g. Skull involvement (↑ hat size), Bowed tibias, kyphosis and fractures
Osteoblasts release Alkaline Phosphatase
(ALP) from the bone into the blood
↑ serum ALP
marker of bone formation
Disorganized bone remodelling, lytic lesion expansion, fracture and bowing of bone all stimulate nociceptive nerve endings on the periosteum
Bone pain
(dull, often night-time)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published November 26, 2012 on www.thecalgaryguide.com