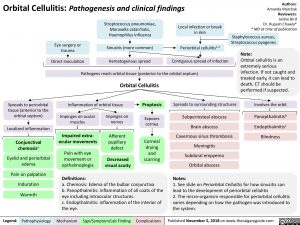
Orbital Cellulitis: Pathogenesis and clinical findings
Authors: Amanda Marchak Reviewers: Jaimie Bird Dr. Rupesh Chawla* * MD at time of publication
Staphylococcus aureus, Streptococcus pyogenes
Note:
Orbital cellulitis is an extremely serious infection. If not caught and treated early, it can lead to death. CT should be performed if suspected.
Involves the orbit
Panopthalmitisb Endopthalmitisc Blindness
Streptococcus pneumoniae, Moraxella catarrhalis, Haemophilus influenza
Local infection or break in skin
Eye surgery or trauma
Direct inoculation
Sinusitis (more common) Periorbital cellulitis1,2
Hematogenous spread
Contiguous spread of infection
Pathogens reach orbital tissue (posterior to the orbital septum)
Spreads to periorbital tissue (anterior to the orbital septum)
Localized inflammation
Conjunctival chemosisa
Eyelid and periorbital edema
Pain on palpation
Induration
Warmth
Orbital Cellulitis Inflammation of orbital tissue Proptosis
Spreads to surrounding structures
Subperiosteal abscess Brain abscess Cavernous sinus thrombosis Meningitis Subdural empyema Orbital abscess
Notes:
Impinges on ocular muscles
Impaired extra- ocular movements
Pain with eye
movement or opthalmoplegia
Definitions:
Impinges on nerves
Afferent pupillary defect
Decreased visual acuity
Exposes cornea
Corneal drying and scarring
a. Chemosis: Edema of the bulbar conjunctiva
b. Panopthalmitis: inflammation of all coats of the eye including intraocular structures.
c. Endopthalmitis: inflammation of the interior of the eye.
1. See slide on Periorbital Cellulitis for how sinusitis can lead to the development of periorbital cellulitis
2. The micro-organism responsible for periorbital cellulitis varies depending on how the pathogen was introduced to the system.
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published November 5, 2018 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Pediatrics Common Pediatric Infections Orbital Cellulitis: Pathogenesis and Clinical Findings Orbital Cellulitis: Pathogenesis and clinical findings