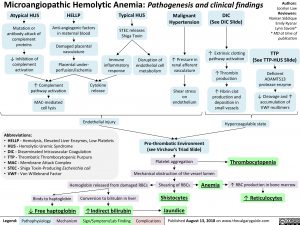
Microangiopathic Hemolytic Anemia: Pathogenesis and clinical findings
Authors: Jocelyn Law Reviewers: Naman Siddique Emily Ryznar Lynn Savoie* * MD at time of publication
Atypical HUS
Mutation or antibody attack of
complement proteins
HELLP
Anti-angiogenic factors in maternal blood
Damaged placental vasculature
Typical HUS
STEC releases Shiga Toxin
Malignant Hypertension
DIC
(See DIC Slide)
↓ Inhibition of complement
Immune inflammatory
↑ Pressure in
↑ Extrinsic clotting pathway activation
TTP
(See TTP-HUS Slide)
Disruption of
endothelial cell
activation perfusion/ischemia response metabolism vasculature ↑Thrombin Deficient
Placental under-
renal afferent
↑ Complement pathway activation
MAC-mediated cell lysis
Cytokine release
Endothelial injury
Shear stress on endothelium
production
↑ Fibrin clot production and deposition in small vessels
ADAMTS13 protease enzyme
↓ Cleavage and ↑ accumulation of VWF multimers
Abbreviations:
• HELLP – Hemolysis, Elevated Liver Enzymes, Low Platelets • HUS – Hemolytic-Uremic Syndrome
• DIC – Disseminated Intravascular Coagulation
• TTP – Thrombotic Thrombocytopenic Purpura
• MAC – Membrane Attack Complex
• STEC – Shiga Toxin-Producing Escherichia coli
• VWF – Von Willebrand Factor
Pro-thrombotic Environment (see Virchow’s Triad Slide)
Platelet aggregation Mechanical obstruction of the vessel lumen
Hypercoagulable state
Thrombocytopenia
↑ RBC production in bone marrow
↑ Reticulocytes
Hemoglobin released from damaged RBCs Shearing of RBCs Anemia
Binds to haptoglobin Conversion to bilirubin in liver
↓ Free haptoglobin ↑Indirect bilirubin
Shistocytes Jaundice
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published August 13, 2018 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Hematology Normocytic Anemias Microangiopathic Hemolytic Anemia: Pathogenesis and clinical findings Microangiopathic Hemolytic Anemia: Pathogenesis and clinical findings