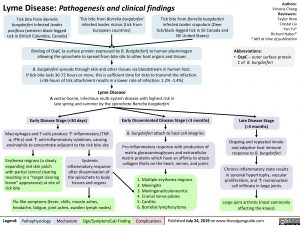
Lyme Disease: Pathogenesis and clinical findings
Authors: Victoria Chang Reviewers: Taylor Woo Crystal Liu Yan Yu* Richard Haber* * MD at time of publication
Abbreviations:
• OspC – outer surface protein
C of B. burgdorferi
Tick bite from Borrelia burgdorferi infected Ixodes pacificus (western black-legged tick in British Columbia, Canada)
Tick bite from Borrelia burgdorferi infected Ixodes ricinus (tick from European countries)
Tick bite from Borrelia burgdorferi infected Ixodes scapularis (Deer tick/black-legged tick in SE Canada and NE United States)
Binding of OspC (a surface protein expressed by B. Burgdorferi) to human plasminogen allowing the spirochete to spread from bite site to other host organs and tissues
B. burgdorferi spreads through skin and other tissues via bloodstream in human host.
If tick bite lasts 36-72 hours or more, this is sufficient time for ticks to transmit the infection. (<36 hours of tick attachment results in a lower rate of infection: 1.2% -1.4%)
Lyme Disease
A vector-borne, infectious multi-system disease with highest risk in late spring and summer by the spirochete Borrelia burgdorferi
Early Disease Stage (<30 days)
Macrophages and T-cells produce ↑ inflammatory (TNF- α, IFN-γ) and ↑ anti-inflammatory cytokines, causing eosinophils to concentrate adjacent to the tick bite site
Early Disseminated Disease Stage (<3 months)
B. burgdorferi attach to host cell integrins
Pro-inflammatory response with production of matrix glycosaminoglycans and extracellular matrix proteins which have an affinity to attack collagen fibrils on the heart, nerves, and joints
1. Multiple erythema migrans 2. Meningitis
3. Meningoradiculoneuritis
4. Cranial nerve palsies
5. Carditis
6. Borrelial lymphocytoma
Late Disease Stage (>3 months)
Ongoing and repeated innate and adaptive host immune response to B. burgdorferi
Chronic inflammatory state results in synovial hypertrophy, vascular
proliferation, and ↑ mononuclear cell infiltrate in large joints
Large joint arthritis (most commonly affecting the knees)
Erythema migrans (a slowly expanding red skin patch with partial central clearing resulting in a “target clearing lesion” appearance) at site of tick bite
Systemic inflammatory response
after dissemination of the spirochete to body tissues and organs
Flu-like symptoms (fever, chills, muscle aches, headache, fatigue, joint aches, swollen lymph nodes)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published July 24, 2019 on www.thecalgaryguide.com
References
• David A. Wetter and Colin A. Ruff. CMAJ August 09, 2011 183 (11) 1281; DOI: https://doi.org/10.1503/cmaj.101533
• https://www.canada.ca/en/public-health/services/diseases/lyme-disease/causes-lyme-disease.html
• Borrelia burgdorferi Infection-Associated Surface Proteins ErpP, ErpA, and ErpC Bind Human Plasminogen. Catherine A. Brissette, Katrin Haupt, Diana Barthel, Anne E. Cooley, Amy Bowman, Christina Skerka, Reinhard Wallich, Peter F. Zipfel, Peter Kraiczy, Brian Stevenson. Infection and Immunity Dec 2008, 77 (1) 300-306; DOI: 10.1128/IAI.01133-08
• https://www.uptodate.com/contents/what-to-do-after-a-tick-bite-to-prevent-lyme-disease-beyond- the-basics
• Murray, T. S., & Shapiro, E. D. (2010). Lyme disease. Clinics in laboratory medicine, 30(1), 311–328. doi:10.1016/j.cll.2010.01.003
• Weedon, David. Weedon’s Skin Pathology E-Book: Expert Consult-Online and Print. Elsevier Health Sciences, 2009.