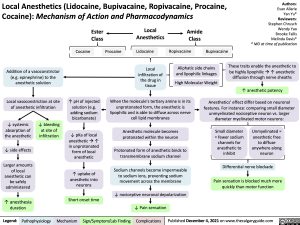
Local Anesthetics (Lidocaine, Bupivacaine, Ropivacaine, Procaine, Cocaine): Mechanism of Action and Pharmacodynamics
Ester Class
Cocaine
Local Anesthetics
Lidocaine
Local infiltration of the drug in tissue
Amide Class
Ropivacaine
Authors: Evan Allarie Yan Yu* Reviewers: Stephen Chrusch Wendy Yao Brooke Fallis Melinda Davis* * MD at time of publication
These traits enable the anesthetic to be highly lipophilicà↑ anesthetic diffusion through nerve sheaths
↑ anesthetic potency
Anesthetics’ effect differ based on neuronal features. For instance: comparing small diameter
unmyelinated nociceptive neuron vs. larger diameter myelinated motor neurons:
Procaine
Bupivacaine
Addition of a vasoconstrictor (e.g. epinephrine) to the anesthetic solution
Local vasoconstriction at site of anesthetic infiltration
Aliphatic side chains and lipophilic linkages
High Molecular Weight
↓ systemic absorption of the anesthetic
↓ side effects Larger amounts
of local anesthetic can be safely administered
↑ anesthesia duration
↓ bleeding at site of infiltration
↑ pH of injected solution (e.g. adding sodium bicarbonate)
↓ pKa of local anestheticà↑ in unprotonated form of local anesthetic
↑ uptake of anesthetic into neurons
Short onset time
When the molecule’s tertiary amine is in its unprotonated form, the anesthetic is lipophilic and is able to diffuse across nerve cell lipid membranes
Anesthetic molecule becomes protonated within the neuron
Protonated form of anesthetic binds to transmembrane sodium channel
Sodium channels become impermeable to sodium ions, preventing sodium movement across the membrane
↓ nociceptive neuronal depolarization ↓ Pain sensation
Small diameter = fewer sodium channels for anesthetic to inhibit
Unmyelinated = anesthetic free
to diffuse anywhere along neuron
Differential nerve blockade
Pain sensation is blocked much more quickly than motor function
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published December 4, 2021 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Anesthesia Drug Mechanisms of Action Local Anesthetics (Lidocaine, Bupivacaine, Ropivacaine, Procaine, Cocaine): Pharmacodynamics local-anesthetics-lidocaine-bupivacaine-ropivacaine-procaine-cocaine-mechanism-of-action-and-pharmacodynamics