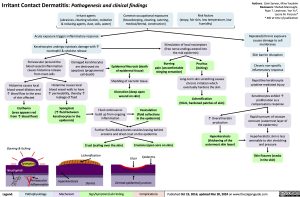
Irritant Contact Dermatitis: Pathogenesis and clinical findings
Authors: Zaini Sarwar, Mina Youakim Reviewers: Shahab Marzoughi, Ryan T. Lewinson, Yan Yu*, Laurie M. Parsons* * MD at time of publication
Repeated/chronic exposure causes damage to cell membranes
Skin barrier disruption
Chronic non-specific inflammatory response
Repetitive keratinocyte cytokine-mediated injury
Keratinocytes exhibit ↑ proliferation as a compensatory response
Rapid turnover of stratum corneum (outermost layer of the epidermis)
Hyperkeratotic skin is less amenable to skin stretching and pressure
Skin fissures (cracks in the skin)
Irritant agents
(abrasives, cleaning solution, oxidative & reducing agents, dust, soils, water)
Acute exposure triggers inflammatory response
Keratinocytes undergo cytotoxic damage with ↑ neutrophil & cytokine release
Common occupational exposures (housekeeping, cleaning, catering, medical/dental, construction)
Risk factors
(atopy, fair skin, low temperature, low humidity)
Stimulation of local nociceptors (free nerve endings extend into the mid epidermis)
Perivascular (around the blood vessel) inflammation causes histamine release from mast cells
Damaged keratinocytes are destroyed via
apoptosis (programmed cell death)
Epidermal Necrosis (death of epidermal tissue)
Shedding of necrotic tissue
Ulceration (deep open wound on skin)
Burning
pain (uncomfortable stinging sensation)
Pruritus (itching)
Histamine causes local blood vessel dilation and ↑ blood flow to the area of skin affected
Erythema (area appears red from ↑ blood flow)
Burning & Itching Spongiosis
Neutrophils Neutrophils
Histamine causes local blood vessel walls to have
↑ permeability, thereby ↑ leakage of fluid
Spongiosis
(↑ fluid between keratinocytes in the epidermis)
Fluid continues to build up from ongoing inflammation
Vesiculation (fluid collections in the epidermis)
Long-term skin scratching causes chronic irritation which eventually hardens the skin
Lichenification
(thick, hardened patches of skin)
↑ Overall keratin production
Hyperkeratosis (thickening of the outermost skin layer)
Further fluid buildup bursts vesicles leaving behind erosions and dried crust on the epidermis
Crust (scaling over the skin)
Lichenification
Erosions (open sore on skin)
Ulcer
Epidermis
Perivascular Inflammation
Hyperkeratosis
Dermis
Dermal-epidermal junction
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published Oct 19, 2016; updated Mar 30, 2024 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Dermatology Eczematous Skin Lesions Irritant Contact Dermatitis: Pathogenesis and Clinical Findings Irritant Contact Dermatitis Pathogenesis and Clinical Findings