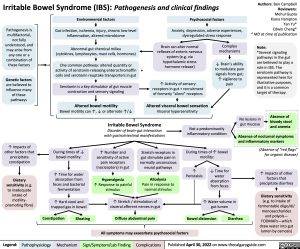
Irritable Bowel Syndrome (IBS): Pathogenesis and clinical findings
Authors: Ben Campbell Reviewers: Mehul Gupta Kiana Hampton Yan Yu* Edwin Cheng* * MD at time of publication
Note:
*Several signaling pathways in the gut are believed to play a role in IBS. The serotonin pathway is represented here for illustrative purposes, and it is a common target of therapy.
Pathogenesis is multifactorial, not fully understood, and may arise from any one or a combination of these factors
Genetic factors
are believed to influence many of these pathways
Environmental factors
Gut infection, ischemia, injury, chronic low-level inflammation, altered microbiome
Abnormal gut chemical milieu (cytokines, lymphocytes, mast cells, hormones)
One common pathway: altered quantity or activity of serotonin-releasing enterochromaffin * cells and serotonin reuptake transporters in gut
Serotonin is a key stimulator of gut muscle contraction and sensory signaling
Altered bowel motility
Bowel motility can ↑, ↓ or alternate ↑/↓
Psychosocial factors
Anxiety, depression, adverse experiences, dysregulated stress response
Brain can alter normal reflexes of enteric nervous system (e.g. via hypothalamic stress hormone release)
↑ Activity of sensory receptors in gut + recruitment of formerly ”silent” receptors
Altered visceral bowel sensation
Visceral hypersensitivity
Complex mechanisms
↓ Brain’s ability to modulate pain signals from gut;
↑ vigilance to pain
Irritable Bowel Syndrome
Disorder of brain-gut interaction with gastrointestinal manifestations
Not a predominantly inflammatory condition
During times of ↑ bowel motility:
No lesions in gut mucosa
(Absence of ”red flags” for organic disease)
↑ Impacts of other factors that precipitate diarrhea
Dietary sensitivity
(e.g. to intake of fermentable oligo/di/ monosaccharides and polyols— FODMAPs—which draw water into gut lumen by osmosis)
↑ Impacts of other factors that precipitate constipation
Dietary sensitivity (e.g. to inadequate intake of motility- promoting fibre)
During times of ↓ bowel motility:
↑ Time for water absorption from feces and bacterial fermentation
↑ Hard stool and trapped gas in bowel
↑ Number and sensitivity of active pain receptors (nociceptors) in gut
Hyperalgesia
↑ Response to painful stimulus
Stretch receptors in gut stimulate pain in normally unconscious neural pathways
Allodynia
Pain in response to normal stimulus
↑ Peristalsis
↓ Time for water absorption from feces
↑ Water volume in gut lumen
↑ Stretch / stimulation of visceral afferent nerves in gut
Absence of bloody stool and anemia
Absence of nocturnal symptoms and inflammatory markers
Constipation
Bloating
Diffuse abdominal pain
All symptoms may exacerbate psychosocial factors
Bowel distension
Diarrhea
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published April 30, 2022 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Gastroenterology Chronic Abdominal Pain Irritable Bowel Syndrome (IBS): Pathogenesis and clinical findings irritable-bowel-syndrome-ibs-pathogenesis-and-clinical-findings