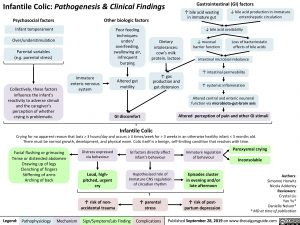
Infantile Colic: Pathogenesis & Clinical Findings
Gastrointestinal (GI) factors
↑ bile acid wasting ↓ bile acid production in immature in immature gut enterohepatic circulation
↓ bile acid availability
Psychosocial factors
Infant temperament Over/understimulation
Parental variables (e.g. parental stress)
Collectively, these factors influence the infant’s reactivity to adverse stimuli and the caregiver’s perception of whether crying is problematic.
Other biologic factors
Poor feeding techniques: under/ overfeeding, swallowing air, infrequent burping
Altered gut motility
GI discomfort
Infantile Colic
Dietary intolerances: cow’s milk protein, lactose
↑ gas production and gut distension
↓ mucosal barrier function
Loss of bacteriostatic effects of bile acids
Immature enteric nervous system
Intestinal microbial imbalance
↑ intestinal permeability
↑ systemic inflammation
Altered central and enteric neuronal function via microbiota-gut-brain axis
Altered perception of pain and other GI stimuli
Crying for no apparent reason that lasts > 3 hours/day and occurs ≥ 3 times/week for > 3 weeks in an otherwise healthy infant < 3 months old. There must be normal growth, development, and physical exam. Colic itself is a benign, self-limiting condition that resolves with time.
Facial flushing or grimacing Tense or distended abdomen
Drawing up of legs Clenching of fingers Stiffening of arms Arching of back
Distress expressed via behaviour
Loud, high- pitched, urgent cry
↑ risk of non- accidental trauma
GI factors directly affect infant’s behaviour
Hypothesized role of immature CNS regulation of circadian rhythm
↑ parental stress
Immature regulation of behaviour
Episodes cluster in evening and/or late afternoon
↑ risk of post- partum depression
Paroxysmal crying Inconsolable
Authors: Simonne Horwitz Nicola Adderley Reviewers: Crystal Liu Yan Yu* Danielle Nelson* * MD at time of publication
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published September 28, 2019 on www.thecalgaryguide.com