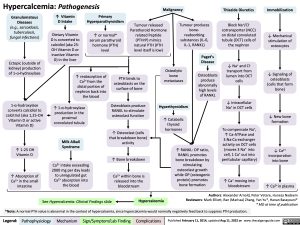
Hypercalcemia: Pathogenesis
Malignancy
Thiazide Diuretics
Immobilization
Granulomatous Diseases (e.g., sarcoidosis, tuberculosis, fungal infections)
Ectopic (outside of kidney) production of 1-α-hydroxylase
1-α-hydroxylase converts calcidiol to calcitriol (aka 1,25-OH Vitamin D or active Vitamin D)
↑ 1-25 OH Vitamin D
↑ Absorption of Ca2+ in the small intestine
↑ Vitamin D Intake
Dietary Vitamin D is converted to calcidiol (aka 25- OH Vitamin D or inactive Vitamin D) in the liver
Primary Hyperparathyroidism
↑ or normal* serum parathyroid hormone (PTH) level
Tumour released Parathyroid Hormone related Peptide (PTHrP) mimics natural PTH (PTH level itself is low)
Tumour produces bone- reabsorbing substances (IL-6, IL-1, RANKL)
Paget’s Disease
Osteoblasts produce abnormally high levels of RANKL
Block Na+/Cl- cotransporter (NCC) on distal convoluted tubule (DCT) cells of the nephron
↓ Na+ and Cl- transport from lumen into DCT cells
↓ Intracellular Na+ in DCT cells
+ To compensate Na ,
↑ Ca-ATPase and 3:Na:Ca exchanger activity on DCT cells (moves 3 Na+ into cell, 1 Ca+ out into peritubular capillary)
↑ Ca+ moving into bloodstream
↓ Mechanical stimulation of osteocytes
↓ Signaling of osteoblasts (cells that form bone)
↓ New bone formation
↓ Ca2+ incorporation
into bone
↑ Ca2+ in plasma
↑ reabsorption of Ca2+ from the distal portion of nephron back into the blood
↑ 1-α-hydroxylase production in the proximal convoluted tubule
Milk Alkali Syndrome
Ca2+ intake exceeding 2000 mg per day leads to unregulated gut Ca2+ absorption into the blood
PTH binds to osteoblasts on the surface of bone
Osteoblasts produce RANKL to stimulate osteoclast function
↑ Osteoclast (cells that breakdown bone) activity
↑ Bone breakdown
Ca2+ within bone is released into the bloodstream
Osteolytic bone metastases
Hyperthyroidism
↑ Catabolic thyroid hormones
↑ RANKL: OP ratio, RANKL promotes bone breakdown by stimulating osteoclast growth while OP (osteogenic protein) promotes bone formation
Hypercalcemia Hypercalcemia
Authors: Alexander Arnold, Peter Vetere, Huneza Nadeem Reviewers: Mark Elliott, Ran (Marissa) Zhang, Yan Yu*, Hanan Bassyouni* * MD at time of publication
See Hypercalcemia: Clinical Findings slide
*Note: A normal PTH value is abnormal in the context of hypercalcemia, since hypercalcemia would normally negatively feed back to suppress PTH production.
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published February 11, 2014, updated Aug 11, 2022 on www.thecalgaryguide.com