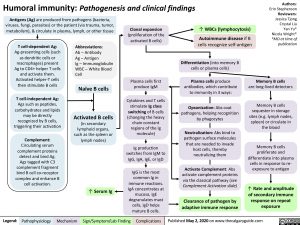
Humoral immunity: Pathogenesis and clinical findings
Authors: Erin Stephenson Reviewers: Jessica Tjong Crystal Liu Yan Yu* Nicola Wright* *MD at time of publication
Memory B cells
are long-lived detectors
Memory B cells sequester in storage sites (e.g. lymph nodes, spleen) or circulate in the blood
Memory B cells proliferate and differentiate into plasma cells in response to re- exposure to antigen
↑ Rate and amplitude of secondary immune response on repeat exposure
Antigens (Ag) are produced from pathogens (bacteria, viruses, fungi, parasites) or the patient (via trauma, tumor, metabolism), & circulate in plasma, lymph, or other tissue
Clonal expansion
(proliferation of the activated B cells)
↑ WBCs (lymphocytosis) Autoimmune disease if B
cells recognize self-antigen
T cell-dependent Ag:
Ag-presenting cells (such as dendritic cells or macrophages) present Ag to CD4+ helper T cells and activate them. Activated helper-T cells then stimulate B cells
T cell-independent Ag:
Ags such as peptides, carbohydrates and lipids
may be directly recognized by B cells, triggering their activation
Complement:
Circulating serum complement proteins detect and bind Ag. Ags tagged with C3 complement fragment bind B cell co-receptor complex and enhance B cell activation.
Abbreviations:
Ab – Antibody
Ag – Antigen
Ig – Immunoglobulin WBC – White Blood Cell
Naïve B cells
Activated B cells
(in secondary lymphoid organs, such as the spleen or lymph nodes)
Plasma cells first produce IgM
Cytokines and T cells stimulate Ig class switching of B cells (changing the heavy chain constant regions of the Ig molecule)
Ig production switches from IgM to IgG, IgA, IgE, or IgD
IgG is the most common Ig in immune reactions. IgA concentrates at mucosa, IgE degranulates mast cells, IgD helps mature B cells.
Differentiation (into memory B cells or plasma cells)
Plasma cells produce antibodies, which contribute to immunity in 3 ways:
Opsonization: Abs coat pathogens, helping recognition by phagocytes
Neutralization: Abs bind to pathogen surface molecules that are needed to invade host cells, thereby neutralizing them
Activate Complement: Abs activate complement proteins via the classical pathway (see Complement Activation slide)
Clearance of pathogen by adaptive immune response
↑ Serum Ig
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published May 2, 2020 on www.thecalgaryguide.com