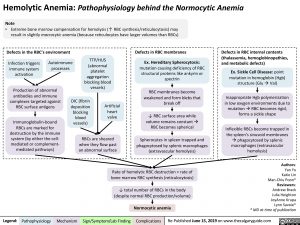
Hemolytic Anemia: Pathophysiology behind the Normocytic Anemia
Note
• Extreme bone marrow compensation for hemolysis (↑ RBC synthesis/reticulocytosis) may result in slightly macrocytic anemia (because reticulocytes have larger volumes than RBCs)
Defects in the RBC’s environment
Defects in RBC membranes
Ex. Hereditary Spherocytosis:
mutation causing deficiency of RBC structural proteins like ankyrin or spectrin
RBC membranes become weakened and form blebs that break off
↓ RBC surface area while volume remains constantà RBC becomes spherical
Spherocytes in spleen trapped and phagocytosed by splenic macrophages (extravascular hemolysis)
Defects in RBC internal contents (thalassemia, hemoglobinopathies, and metabolic defects)
Ex. Sickle Cell Disease: point mutation in hemoglobin (Hgb) structure (GluàVal)
Inappropriate Hgb polymerization in low oxygen environments due to mutationàRBC becomes rigid, forms a sickle shape
Inflexible RBCs become trapped in the spleen’s sinusoid membranes àphagocytosed by splenic macrophages (extravascular hemolysis)
Infection triggers immune system activation
Autoimmune processes
TTP/HUS (abnormal platelet aggregation blocking blood vessels)
Production of abnormal
antibodies and immune complexes targeted against RBC surface antigens
Immunoglobulin-bound RBCs are marked for
destruction by the immune system (by either the cell- mediated or complement- mediated pathways)
DIC (fibrin deposition blocking blood vessels)
Artificial heart valve
RBCs are sheared when they flow past an abnormal surface
Rate of hemolytic RBC destruction > rate of bone marrow RBC synthesis (reticulocytosis)
↓ total number of RBCs in the body (despite normal RBC production/volume)
Normocytic anemia
Authors: Yan Yu Katie Lin Man-Chiu Poon* Reviewers: Andrew Brack Julia Heighton JoyAnne Krupa Lynn Savoie* * MD at time of publication
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-Published June 15, 2019 on www.thecalgaryguide.com