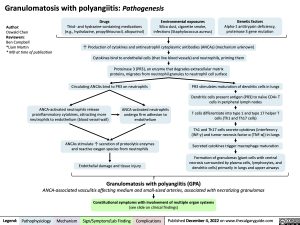
Granulomatosis with polyangiitis: Pathogenesis
Author:
Oswald Chen
Reviewers:
Ben Campbell
*Liam Martin
* MD at time of publication
Drugs
Thiol- and hydrazine-containing medications (e.g., hydralazine, propylthiouracil, allopurinol)
Environmental exposures
Silica dust, cigarette smoke, infections (Staphylococcus aureus)
Genetic factors
Alpha-1 antitrypsin deficiency, proteinase 3 gene mutation
↑ Production of cytokines and antineutrophil cytoplasmic antibodies (ANCAs) (mechanism unknown) Cytokines bind to endothelial cells (that line blood vessels) and neutrophils, priming them
Proteinase 3 (PR3), an enzyme that degrades extracellular matrix proteins, migrates from neutrophil granules to neutrophil cell surface
Circulating ANCAs bind to PR3 on neutrophils
PR3 stimulates maturation of dendritic cells in lungs
Dendritic cells present antigen (PR3) to naïve CD4+ T cells in peripheral lymph nodes
T cells differentiate into type 1 and type 17 helper T cells (Th1 and Th17 cells)
Th1 and Th17 cells secrete cytokines (interferon γ (INF-γ) and tumor necrosis factor α (TNF-α)) in lungs
Secreted cytokines trigger macrophage maturation
Formation of granulomas (giant cells with central necrosis surrounded by plasma cells, lymphocytes, and dendritic cells) primarily in lungs and upper airways
ANCA-activated neutrophils release proinflammatory cytokines, attracting more neutrophils to endothelium (blood vessel wall)
ANCA-activated neutrophils undergo firm adhesion to endothelium
ANCAs stimulate ↑ secretion of proteolytic enzymes and reactive oxygen species from neutrophils
Endothelial damage and tissue injury
Granulomatosis with polyangiitis (GPA)
ANCA-associated vasculitis affecting medium and small-sized arteries, associated with necrotizing granulomas
Constitutional symptoms with involvement of multiple organ systems
(see slide on clinical findings)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published December 4, 2022 on www.thecalgaryguide.com
Granulomatosis with polyangiitis: Clinical findings Inflammation-mediated endothelial damage and granuloma formation
(see slide on pathogenesis)
Granulomatosis with polyangiitis (GPA)
Author:
Oswald Chen
Reviewers:
Ben Campbell
*Liam Martin
* MD at time of publication
ANCA-associated vasculitis affecting medium and small-sized arteries, associated with necrotizing granulomas
Constitutional symptoms
Fever, unintentional weight loss, night sweats, arthralgias
Skin involvement
Inflammation of cutaneous vessels
Systemic inflammation obstructing blood flow, with granulomatous lesions primarily in upper airways and lungs
Ear, nose, and throat involvement
↑ C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) (markers of inflammation)
Necrotizing granulomas on biopsy of affected tissue
Positive PR3-ANCA/c-ANCA blood test (antibodies present in ~90% of patients, described in GPA Pathogenesis slide)
Renal involvement
Inflammation of renal vessels
Rupture of basement membrane (layer that filters blood from glomerular capillaries into Bowman’s capsule)
Pauci-immune glomerulonephritis (see Nephritic Syndrome slide)
Rapidly progressive glomerulonephritis
Eye involvement
Inflammation of ocular tissue
Conjunctivitis
Scleritis/ episcleritis (painful red eye)
Lower respiratory tract involvement
Inflammation of pulmonary vessels
Vessel occlusion and ischemia
Skin necrosis
Vessels burst and blood pools under skin
Round and retiform (net- like) palpable purpura of lower extremities
Granulomatous destruction of nasal cartilage
Collapse of nasal bridge
Saddle nose deformity
Inflammation of paranasal sinus and nasal cavity vessels
↓ Perfusion of lungs
Dyspnea
Damage to interstitial capillaries
Hemoptysis
Diffuse alveolar hemorrhage
Rhinitis/ sinusitis
Granulomatous obstruction of eustachian tube
Otitis media (see Otitis Media slide)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published December 4, 2022 on www.thecalgaryguide.com