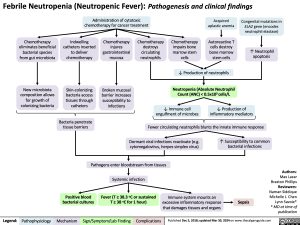
Febrile Neutropenia (Neutropenic Fever): Pathogenesis and clinical findings
Administration of cytotoxic chemotherapy for cancer treatment
Acquired aplastic anemia
Autoreactive T cells destroy bone marrow stem cells
Congenital mutations in ELA2 gene (encodes neutrophil elastase)
↑ Neutrophil apoptosis
Chemotherapy eliminates beneficial bacterial species from gut microbiota
New microbiota composition allows for growth of colonizing bacteria
Indwelling catheters inserted to deliver chemotherapy
Skin-colonizing bacteria access tissues through catheters
Bacteria penetrate tissue barriers
Chemotherapy injures gastrointestinal mucosa
Broken mucosal barrier increases susceptibility to infections
Chemotherapy destroys circulating neutrophils
Chemotherapy impairs bone marrow stem cells
↓ Production of neutrophils
Neutropenia (Absolute Neutrophil Count (ANC) < 0.5x109 cells/L
↓ Immune cell ↓ Production of engulfment of microbes inflammatory mediators
Fewer circulating neutrophils blunts the innate immune response
Pathogens enter bloodstream from tissues Systemic infection
Authors: Max Lazar Braxton Phillips Reviewers: Naman Siddique Michelle J. Chen Lynn Savoie* * MD at time of publication
Dormant viral infections reactivate (e.g. cytomegalovirus, herpes simplex virus)
↑ Susceptibility to common bacterial infections
Positive blood bacterial cultures
Fever (T ≥ 38.3 oC or sustained T ≥ 38 oC for 1 hour)
Immune system mounts an excessive inflammatory response that damages tissues and organs
Sepsis
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published Dec 5, 2018; updated Mar 30, 2024 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Hematology Neutropenia Febrile Neutropenia: Pathogenesis and clinical findings Febrile Neutropenia Pathogenesis and clinical findings