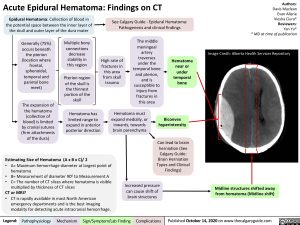
Acute Epidural Hematoma: Findings on CT
Authors: Davis Maclean Evan Allarie Viesha Ciura* Reviewers: Yan Yu* * MD at time of publication
Image Credit: Alberta Health Services Repository
Epidural Hematoma: Collection of blood in the potential space between the inner layer of the skull and outer layer of the dura mater
See Calgary Guide – Epidural Hematoma: Pathogenesis and clinical findings
Generally (75%) occurs beneath
the pterion (location where frontal, sphenoidal, temporal and parietal bone meet)
The expansion of the hematoma (collection of blood) is limited by cranial sutures (firm attachments of the dura)
Multiple bony connections
decrease stability in this region
Pterion region of the skull is
the thinnest portion of the skull
Hematoma has limited range to expand in anterior posterior direction
High rate of fractures in this area from skull trauma
The middle meningeal artery traverses under the temporal bone and pterion, and is susceptible to injury from fractures in this area
Hematoma near or under temporal bone
Hematoma must expand medially, or
inwards, towards brain parenchyma
Biconvex hyperintensity
Can lead to brain herniation (See Calgary Guide: Brain Herniation Types and Clinical Findings)
Estimating Size of Hematoma (A x B x C)/ 2
• A= Maximum hemorrhage diameter at largest point of hematoma
• B= Measurement of diameter 900 to Measurement A
• C= The number of CT slices where hematoma is visible
multiplied by thickness of CT slices
CT or MRI?
• CT is rapidly available in most North American emergency departments and is the best imaging modality for detecting acute intracranial hemorrhage.
Increased pressure can cause shift of brain structures
Midline structures shifted away from hematoma (Midline shift)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published October 14, 2020 on www.thecalgaryguide.com