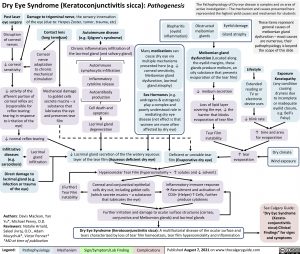
Dry Eye Syndrome (Keratoconjunctivitis sicca): Pathogenesis
The Pathophysiology of Dry eye disease is complex and an area of active investigation – The mechanism and causes presented here represented the highest yield causes and mechanism for students
Post laser eye surgery
Disruption of corneal nerves
↓ corneal sensitivity
Damage to trigeminal nerve, the sensory innervation of the eye (due to: Herpes Zoster, tumor, trauma, etc)
Blepharitis (eyelid inflammation)
Many medications can cause dry eye via
multiple mechanisms presented here (e.g. ↓ corneal sensitivity, Meibomian gland dysfunction, lacrimal gland atrophy)
Sex Hormones (e.g. androgens & estrogens) play a complex and poorly understood role in mediating dry eye disease (net effect is that women are more often affected by dry eye)
Obstructed meibomian glands
Eyelid damage Gland atrophy
These items represent general causes of meibomian gland dysfunction – exact causes are numerous, their pathophysiology is beyond the scope of this slide
Contact lens (long term use)
Corneal nerve adaptation to chronic mechanical stimulation
Autoimmune disease (e.g. Sjögren’s syndrome)
Chronic inflammatory infiltration of the lacrimal gland (and salivary gland)
Autoimmune Lymphocytic infiltration
Inflammatory cytokine release
Autoantibody production
Cell death and apoptosis
Lacrimal gland degeneration
Meibomian gland dysfunction (Located along the eyelid margins, these glands produce meibum, an oily substance that prevents evaporation of the tear film)
↓ meibum secretion Loss of lipid layer
covering the eye, ↓ the barrier that blocks evaporation of tear film
Tear Film instability
Lifestyle
Extended reading or
TV or electronic device uses
Exposure Keratopathy (any condition causing dryness due to incomplete or inadequate eyelid closure, e.g. Bell’s Palsy)
↓ activity of the afferent portion of
corneal reflex arc (responsible for reflex tearing: tearing in response to irritation of the eye)
Mechanical damage to goblet cells
secrete mucins – a substance that lubricates the eye and preserves tear film
↓ blink rate
↑ time and area
↓ normal reflex tearing
for evaporation
Dry climate Wind exposure
Infiltrative diseases
(e.g. sarcoidosis)
Lacrimal gland infiltration
↓ Lacrimal gland secretion of the the watery aqueous layer of the tear film (Aqueous deficient dry eye)
Deficient or unstable tear film (Evaporative dry eye)
↑ tear evaporation
Direct damage to lacrimal gland (e.g. infection or trauma of the eye)
Authors: Davis Maclean, Yan Yu*, Michael Penny, O.D.
Reviewers: Natalie Arnold, Saleel Jivraj, O.D., Adam Muzychuk*, Victor Penner* *MD at time of publication
Hyperosmolar Tear Film (hyperosmolarity = ↑ solutes and ↓ solvent)
(Further) Tear Film instability
Corneal and conjunctival epithelial
cells dry out, including goblet cells (which secrete mucins – a substance that lubricates the eye)
Inflammatory immune response àRecruitment and activation of CD4+ (Helper) T-Cells, further produce cytokines
Further irritation and damage to ocular surface structures (cornea, conjunctiva and Meibomian glands) and lacrimal glands
See Calgary Guide: “Dry Eye Syndrome
(Kerato- conjunctivitis sicca):Clinical Findings” for signs and symptoms
Dry Eye Syndrome (Keratoconjunctivitis sicca): A multifactorial disease of the ocular surface and tears characterized by loss of tear film homeostasis, tear film hyperosmolality and inflammation
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published August 7, 2021 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Ophthalmology Non-Emergent Acute Vision Loss Dry Eye Syndrome: Pathogenesis Dry-Eye-Syndrome-Pathogenesis