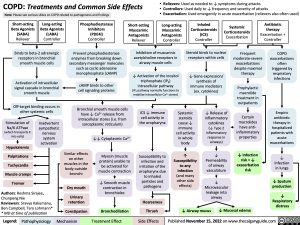
COPD: Treatments and Common Side Effects Note: Please see various slides on COPD related to pathogenesis and findings
• Relievers: Used as needed to ↓ symptoms during attacks
• Controllers: Used daily to ↓ frequency and severity of attacks
• Exacerbation: Used emergently in acute exacerbation (relievers also often used)
Short-acting Beta Agonists (SABA) Reliever
Long-acting Beta Agonists (LABA) Controller
Long-acting Muscarinic Antagonists Controller
Inhaled Corticosteroids (ICS) Controller
Phosphodiesterase Inhibitors (PDE4i) Controller
Short-acting Muscarinic Antagonists Reliever
Systemic Corticosteroids Exacerbation
Antibiotic therapy Exacerbation + Controller
Binds to beta-2 adrenergic receptors in bronchial smooth muscle cells
Activation of intracellular signal cascade in bronchial smooth muscle
Off-target binding occurs in other systemic cells
Prevent phosphodiesterase enzymes from breaking down secondary messenger molecules such as cyclic adenosine monophosphate (cAMP)
cAMP binds to other cell signaling proteins
Bronchial smooth muscle cells have ↓ Ca2+ release from intracellular stores (i.e. from sarcoplasmic reticulum)
Inhibition of muscarinic acetylcholine receptors in airway muscle cells
↓ Activation of the inositol triphosphate (IP3)
intracellular pathway
(IP3 pathway normally functions to mobilize intracellular Ca2+ stores)
Steroid binds to nuclear receptors within cells
↓ Gene expression/ synthesis of immune mediators (ex. cytokines)
Frequent moderate-severe exacerbations despite maximal therapy
Prophylactic macrolide treatment in outpatients
Certain macrolides have anti- inflammatory properties
↓ Infection risk = ↓ exacerbation risk
COPD exacerbations often triggered by respiratory infections
Empiric antibiotic therapy in hospitalized patients with acute exacerbations
↓ Infection in lungs
↓ Sputum production
↓ Respiratory distress
Stimulation of
Na/K ATPase (which transports K into cells)
Hypokalemia Palpitations Tachycardia Muscle cramps Tremor
Inadvertent sympathetic nervous system activation
↓↓ Cytoplasmic Ca2+
Myosin (muscle protein) unable to be activated for muscle contraction
↓ Smooth muscle contraction in bronchioles
Bronchodilation
ICS ↓ immune cell activity in the oropharynx
Susceptibility to infection and irritation of the oropharynx due to inhaled particles and pathogens
Hoarseness Thrush
Systemic steroids cause ↓ immune cell activity in whole body
↑ Susceptibility to any infection (and many other side effects)
↓ Release of inflammatory cytokines (↓ Type 2 inflammatory response in airways)
↓ Permeability of airway vasculature
↓ Microvascular leakage into airway
Authors: Reshma Sirajee, Chunpeng Nie
Reviewers: Sravya Kakumanu, Ben Campbell, Tara Lohmann* * MD at time of publication
Similar effects on other muscles in the body outside bronchi
Dry mouth
Urinary retention
Constipation
↓ Airway mucus ↓ Mucosal edema
Legend:
Pathophysiology
Mechanism
Treatment Effect
Side Effects
Published November 15, 2022 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Respirology Obstructive Lung Disease COPD: Treatments and Common Side Effects COPD: Treatments and Common Side Effects