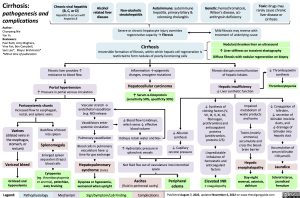
Cirrhosis:
pathogenesis and complications
Author:
Chunpeng Nie
Yan Yu
Reviewers:
Paul Ratti, Amy Maghera, Vina Fan, Ben Campbell,
Sam Lee*, Mayur Brahmania* *MD at time of publication
Chronic viral hepatitis (B, C, or D) Hepatitis D occurs with hepatitis B
Alcohol related liver disease
Non-alcoholic steatohepatitis
Autoimmune: autoimmune hepatitis, primary biliary & sclerosing cholangitis
Genetic: hemochromatosis, Wilson’s disease, α1- antitrypsin deficiency
Toxic: drugs may rarely cause chronic liver disease or cirrhosis
Severe or chronic hepatocyte injury overrides regenerative capacity → Fibrosis
Cirrhosis
Mild fibrosis may reverse with treatment of underlying cause
Nodular/shrunken liver on ultrasound
↑ Liver stiffness on transient elastography Diffuse fibrosis with nodular regeneration on biopsy
Fibrotic liver provides ↑ resistance to blood flow
Portal hypertension
Irreversible formation of fibrosis, within which hepatic cell regeneration is restricted to form nodules of poorly-functioning cells
Inflammation → epigenetic changes, oncogene mutations
Hepatocellular carcinoma
↑ Serum α-fetoprotein (sensitivity 50%, specificity 99%)
Fibrosis disrupts normal function of hepatic lobules
Hepatic insufficiency
↓ Liver synthetic function
↓ Thrombopoietin synthesis
Thrombocytopenia
↓ Conjugation of bilirubin,
↓ secretion of bilirubin into bile ducts, and
↓ drainage of bilirubin into hepatic duct
Accumulation of serum bilirubin >30 μmol/L
Jaundice
Scleral icterus, jaundiced frenulum
↑ Pressure in portal venous circulation
Portosystemic shunts
Increased flow to esophageal, rectal, and splenic veins
Vascular stretch → endothelial vasodilator (e.g. NO) release
Vasodilators enter systemic circulation
Pulmonary vasodilation
Blood cells in pulmonary vasculature have ↓ time for gas exchange
Hepatopulmonary syndrome (rare)
Dyspnea or hypoxemia, worsened when upright
↓ Synthesis of clotting factors (V, VII, IX, X, XI, XII, fibrinogen, prothrombin) and anticoagulant proteins (antithrombin, proteins C/S)
Unpredictable imbalance of hemostatic and anticoagulant factors
Elevated INR
± coagulopathy
Impaired metabolism of waste products and toxins
Toxins (mainly ammonia) accumulate and cross the blood- brain barrier
Hepatic encephalopathy
Day-night reversal, asterixis, delirium
Varices
(dilated veins in the esophagus, stomach, or rectum)
Variceal bleed
GI bleed and hypovolemia
Backflow of blood into spleen
Splenomegaly
Enlarged spleen sequesters (traps) blood cells
Cytopenias
(eg. thrombocytopenia or anemia), petechiae, easy bruising
↓ Blood flow to kidneys, which sense ↓ effective blood volume
Kidneys retain water and Na+
↑ Hydrostatic pressure in splanchnic vessels
↓ Albumin synthesis
↓ Capillary oncotic pressure
Net fluid flux out of vasculature into interstitial space
Ascites
(fluid in peritoneal cavity)
Peripheral edema
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published August 7, 2022, updated November 6, 2022 on www.thecalgaryguide.com