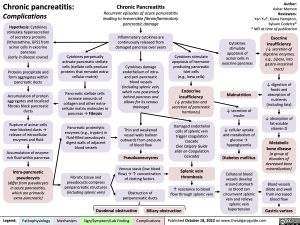
Chronic pancreatitis:
Complications
Hypothesis: Cytokines stimulate hypersecretion of secretory proteins (lithostathine, GP2) from acinar cells in exocrine pancreas
(early in disease course)
Proteins precipitate and form aggregates within pancreatic ducts
Accumulation of protein aggregates and localized fibrosis block pancreatic ducts
Rupture of acinar cells near blocked ducts → release of intracellular enzymes and fluid
Accumulation of enzyme- rich fluid within pancreas
Intra-pancreatic pseudocysts (differ from pseudocysts in acute pancreatitis, which are primarily extra-pancreatic)
Chronic Pancreatitis
Recurrent episodes of acute pancreatitis leading to irreversible fibroinflammatory pancreatic damage
Inflammatory cytokines are
continuously released from damaged pancreas over years
Cytokines damage endothelium of intra- and peri-pancreatic blood vessels (including splenic vein, which runs posteriorly behind pancreas and allows for its venous drainage)
Thin and weakened
vessel walls balloon outwards from pressure of blood flow
Pseudoaneurysms
Venous stasis (low blood flow) → ↑ concentration of clotting factors
Obstruction of peripancreatic ducts
Author: Ashar Memon Reviewers: Yan Yu*, Kiana Hampton, Sylvain Coderre* * MD at time of publication
Exocrine insufficiency
(↓ secretion of digestive enzymes, e.g., Lipase, into gastro-intestinal tract)
↓ digestion of foods and absorption of nutrients (including fats)
↓ absorption of fat-soluble vitamin D
Metabolic bone disease
(a group of disorders of decreased bone mineralization)
Blood vessels dilate and swell from increased blood flow
Gastric varices
Cytokines perpetually activate pancreatic stellate cells (stellate cells produce proteins that remodel extra- cellular matrix)
Pancreatic stellate cells increase amounts of collagen and other extra- cellular matrix molecules in pancreas → Fibrosis
Pancreatic proteolytic enzymes (e.g., trypsin) in fluid-filled pseudocysts digest walls of adjacent blood vessels
Fibrotic tissue and pseudocysts compress peripancreatic structures (including splenic vein)
Cytokines stimulate apoptosis of hormone- producing pancreatic Islet cells
(e.g., beta cells)
Endocrine insufficiency
(↓ production and secretion of pancreatic hormones)
Damaged endothelial cells of splenic vein trigger coagulation cascade
(See Calgary Guide slide on Coagulation Cascade)
Splenic vein thrombosis
↑ resistance to blood flow through splenic vein
Cytokines
stimulate apoptosis of acinar cells in exocrine pancreas
Malnutrition
↓ secretion of insulin
↓ cellular uptake and metabolism of glucose → hyperglycemia
Diabetes mellitus
Collateral blood vessels develop around stomach so blood can circumvent splenic vein and relieve splenic vein hypertension
Duodenal obstruction Biliary obstruction
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published October 18, 2022 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Gastroenterology Acute GI Related Abdominal Pain Chronic pancreatitis: Complications chronic-pancreatitis-complications