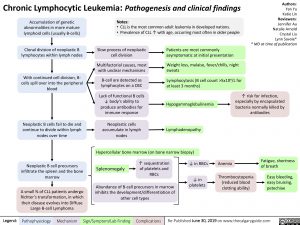
Chronic Lymphocytic Leukemia: Pathogenesis and clinical findings
Authors: Yan Yu Katie Lin Reviewers: Jennifer Au Natalie Arnold Crystal Liu Lynn Savoie* * MD at time of publication
Accumulation of genetic abnormalities in more mature lymphoid cells (usually B-cells)
Clonal division of neoplastic B lymphocytes within lymph nodes
With continued cell division, B- cells spill over into the peripheral blood
Neoplastic B cells fail to die and continue to divide within lymph nodes over time
Neoplastic B cell precursors infiltrate the spleen and the bone marrow
A small % of CLL patients undergo Richter’s transformation, in which their disease evolves into Diffuse Large B-cell Lymphoma
Notes:
• CLL is the most common adult leukemia in developed nations.
• Prevalence of CLL ↑ with age, occurring most often in older people
Slow process of neoplastic cell division
Patients are most commonly asymptomatic at initial presentation
Multifactorial causes, most Weight loss, malaise, fever/chills, night
with unclear mechanisms
B-cell are detected as lymphocytes on a CBC
Lack of functional B cells ↓ body’s ability to produce antibodies for immune response
Neoplastic cells accumulate in lymph nodes
sweats
Lymphocytosis (B cell count >5×109/L for at least 3 months)
Hypogammaglobulinemia
Lymphadenopathy
↑ risk for infection, especially by encapsulated bacteria normally killed by antibodies
Hypercellular bone marrow (on bone narrow biopsy)
Splenomegaly
↑ sequestration of platelets and RBCs
↓ in RBCs ↓ in
platelets
Anemia
Thrombocytopenia (reduced blood clotting ability)
Fatigue, shortness of breath
Easy bleeding, easy bruising, petechiae
Abundance of B-cell precursors in marrow inhibits the development/differentiation of other cell types
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-Published June 30, 2019 on www.thecalgaryguide.com