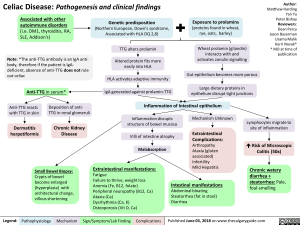
Celiac Disease: Pathogenesis and clinical findings
Associated with other autoimmune disorders (i.e. DM1, thyroiditis, RA, SLE, Addison’s)
Genetic predisposition -■ (Northern European, Down’s syndrome, Associated with HLA DQ 2,8)
Note: *The anti-TTG antibody is an IgA anti-body, therefore if the patient is IgA-deficient, absence of anti-TTG does not rule out celiac
Anti-TTG in serum*
Anti-TTG reacts with TTG in skin
Deposition of anti-TTG in renal glomeruli
Dermatitis herpetiformis
Chronic Kidney Disease
Small Bowel Biopsy: Crypts of bowel become enlarged (hyperplasia) with architectural change, villous shortening
Legend: Pathophysiology
Mechanism
Exposure to prolamins (proteins found in wheat, rye, oats, barley)
TTG alters prolamin Altered protein fits more easily into HLA
HLA activates adaptive immunity
IgA generated against prolamin-TTG
Wheat prolamin (gliandin) interacts with and activates zonulin signalling
Gut epithelium becomes more porous
Large dietary proteins in epithelium disrupt tight junctions
Author: Matthew Harding Yan Yu Peter Bishay Reviewers: Dean Percy Jason Baserman Usama Malik Kerri Novak* * MD at time of publication
Inflammation of Intestinal epithelium Inflammation disrupts structure of bowel mucosa Mechanism Unknown Lymphocytes migrate to site of inflammation Extraintestinal Complications: Arthropathy Ataxia (gluten associated) Infertility Mild Hepatitis Villi of intestine atrophy Risk of Microscopic Colitis (50x) Malabsorption Extraintestinal manifestations: Chronic watery Fatigue Failure to thrive, weight loss Anemia (Fe, B12, folate) Peripheral neuropathy (B12, Ca) Ataxia (Ca) Dysrhythmia (Ca, K) Osteoporosis (Vit D, Ca) diarrhea + Intestinal manifestations steatorrhea: Pale, foul-smelling Abdominal bloating Steatorrhea (fat in stool) Diarrhea