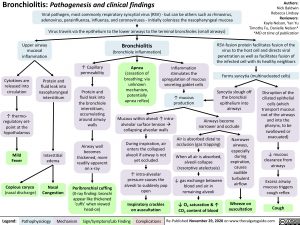
Bronchiolitis: Pathogenesis and clinical findings
Viral pathogen, most commonly respiratory syncytial virus (RSV) – but can be others such as rhinovirus,
adenovirus, parainfluenza, influenza, and coronaviruses – initially colonizes the nasopharyngeal mucosa Virus travels via the epithelium to the lower airways to the terminal bronchioles (small airways)
Authors: Nick Baldwin Rebecca Lindsay Reviewers: Kayla Nelson, Yan Yu Timothy Fu, Danielle Nelson* *MD at time of publication
Upper airway mucosal inflammation
Bronchiolitis
(bronchiole inflammation)
Apnea
(cessation of breathing; via unknown mechanism, potentially apnea reflex)
RSV-fusion protein facilitates fusion of the virus to the host cell and directs viral penetration as well as facilitates fusion of the infected cell with its healthy neighbors
Forms syncytia (multinucleated cells)
Cytokines are released into circulation
↑ thermo- regulatory set- point at the hypothalamus
Mild Fever
Copious coryza
(nasal discharge)
Protein and fluid leak into nasopharyngeal interstitium
↑ Capillary permeability
Protein and fluid leak into the bronchiole interstitium, accumulating around airway walls
Airway wall becomes thickened, more readily apparent on x-ray
Peribronchial cuffing
(X-ray finding: bronchi appear like thickened ‘cuffs’ when viewed head-on)
Inflammation stimulates the upregulation of mucous secreting goblet cells
↑ mucous production
Mucous within alveoli ↑ intra- alveolar surface tensionà collapsing alveolar walls
During inspiration, air enters the collapsed alveoli if airway is not yet occluded
↑ intra-alveolar pressure causes the alveoli to suddenly pop open
Inspiratory crackles on auscultation
Syncytia slough off the bronchial epithelium into airways
Airways become narrower and occlude
Disruption of the ciliated epithelial cells (which transport mucous out of the airways and into the pharynx, to be swallowed or evacuated)
↓ mucous clearance from airways
Excess airway mucous triggers cough reflex
Cough
Interstitial edema
Nasal Congestion
Air is absorbed distal to occlusion (gas trapping)
When all air is absorbed, alveoli collapse (resorptive atelectasis)
↓ gas exchange between blood and air in remaining alveoli
↓ O2 saturation & ↑ CO2 content of blood
Narrower airways, especially during expiration, causes audible turbulent airflow
Wheeze on auscultation
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-Published November 29, 2020 on www.thecalgaryguide.com