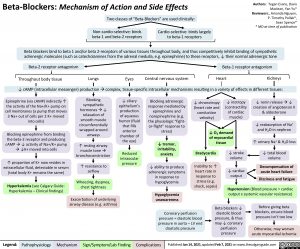
Beta-Blockers: Mechanism of Action and Side Effects Two classes of “Beta-Blockers” are used clinically:
Non-cardio-selective: binds Cardio-selective: binds largely beta-1 and beta-2 receptors to beta-1 receptors
Authors: Tegan Evans, Davis Maclean, Yan Yu* Reviewers:, Amanda Nguyen, P. Timothy Pollak*, Sean Spence* * MD at time of publication
Beta blockers bind to beta 1 and/or beta 2-receptors of various tissues throughout body, and thus competitively inhibit binding of sympathetic adrenergic molecules (such as catecholamines from the adrenal medulla, e.g. epinephrine) to these receptors, ↓ their normal adrenergic tone
Beta-2 receptor antagonism Beta-1 receptor antagonism
Lungs Eyes Central nervous system Heart Kidneys ↓ cAMP (intracellular messenger) productionàcomplex, tissue-specific intracellular mechanisms resulting in a variety of effects in different tissues:
Throughout body tissue
Epinephrine (via cAMP) indirectly ↑ the activity of the Na+/K+ pump on cell membranes (a pump that moves 3 Na+ out of cells per 2 K+ moved into cells)
Blocking epinephrine from binding
the beta-2 receptor and producing cAMPà↓ activity of Na+/K+ pump à↓K+ moved into cells
↑ proportion of K+ now resides in extracellular fluid, detectable in serum (total body K+ remains the same)
Hyperkalemia (see Calgary Guide: Hyperkalemia – Clinical findings)
Blocking sympathetic hormonesà↓ relaxation of smooth muscle circumferentially wrapped around airways
↑ resting airway muscle toneà bronchoconstriction
↑ resistance to airflow
Wheezing, dyspnea, chest tightness
Exacerbation of underlying airway disease (e.g. asthma)
↓ ciliary epithelium’s production of aqueous humor (fluid that fills anterior chamber of the eye)
Reduced intraocular pressure
Blocking adrenergic response mediated by epinephrine and norepinephrine (e.g. the physiologic “fight- or-flight” response to stress)
↓ tremor, irritability, anxiety
↓ ability to produce adrenergic symptoms in response to hypoglycemia
Hypoglycemia unawareness
Coronary perfusion pressure = diastolic blood pressure in aorta – LV end diastolic pressure
↓ inotropy (contractility of cardiac muscle)
↓ chronotropy (heart rate and conduction velocity)
↓ renin releaseà↓ creation of angiotensin II & aldosterone
+ ↓ reabsorption of Na
and H2O in nephron
↑ urinary Na+ & H2O loss
↓ total blood volume
Decompensation of acute heart failure
Dizziness and fatigue Hypotension (Blood pressure = cardiac
output x systemic vascular resistance)
↓ O2 demand of myocardial tissue
Bradycardia
Inability to ↑ heart rate in response to stress (e.g. shock, sepsis)
↓ stroke volume
↓ cardiac output
Beta blockers ↓ diastolic blood pressure, & thus may ↓ coronary perfusion pressure
Before giving beta blockers, ensure blood pressure isn’t too low
Otherwise, may worsen acute myocardial ischemia
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published Jan 14, 2021, updated Feb 7, 2021 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Pharmacology Cardiovascular Beta Blockers: Mechanism of Action and Side Effects Beta-Blockers-Mechanism-of-Action-and-Side-Effects