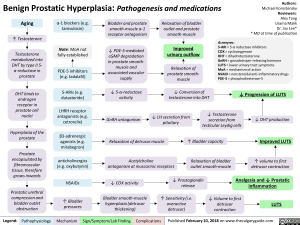
Benign Prostatic Hyperplasia: Pathogenesis and medications
Aging
Testosterone
Testosterone metabolized into DHT by type II 5- a-reductase in prostate
DHT binds to androgen receptor in prostate cell nuclei
Hyperplasia of the prostate
Prostate encapsulated by fibromuscular tissue, therefore grows inwards
Prostatic urethral compression and bladder outlet obstruction
Legend:
a-1 blockers (e.g. tamsulosin)
Note: MoA not fully established
PDE-5 inhibitors (e.g. tadalafil)
Bladder and prostate smooth-muscle a-1 receptor antagonism
—110.
Relaxation of bladder outlet and prostate smooth-muscle
Authors: Michael Korostensky Reviewers: Alex Tang Usama Malik Dr. Jay Lee* * MD at time of publication
Acronyms: 5-ARI = 5-a reductase inhibitors COX = cyclooxygenase DHT = dihydrotestosterone GnRH = gonadotropin-releasing hormone LUTS = lower urinary tract symptoms PDE-5-mediated cGMP degradation in prostate smooth-Improved urinary outflow muscle and associated vascular supply Relaxation of prostate smooth-muscle MoA = mechanism of action NSAID = nonsteroidal anti-inflammatory drugs PDE-5 = phosphodiesterase-5 -NO
5-ARIs (e.g. dutasteride)
LHRH receptor antagonists (e.g. cetrorel ix)
P3-adrenergic agonists (e.g. mirabegron)
anticholinergics (e.g. oxybutynin)
NSAIDs
1` Bladder pressures
Pathophysiology Mechanism
5-a-reductase activity
1, Conversion of testosterone into DHT
4, Progression of LUTS
1, Testosterone secretion from testicular Leydig cells 1, LH secretion from pituitary GnRH antagonism DHT production Relaxation of detrusor Bladder muscle 1` capacity Improved LUTS
Acetylcholine antagonism at muscarinic receptors Relaxation of bladder outlet smooth-muscle 1` volume to first detrusor contraction 4, Prostaglandin release Analgesia and 4, Prostatic ,f, COX activity ► inflammation —110. Bladder smooth-muscle hyperplasia (detrusor thickening) /1` Sensitivity (i.e. overactive detrusor) -1110. 1, Volume to first detrusor contraction LUTS
Foundations
Systems
Other Languages
Urology Prostate Disease Benign Prostatic Hyperplasia: Pathogenesis and medications Benign Prostatic Hyperplasia: Pathogenesis and medications