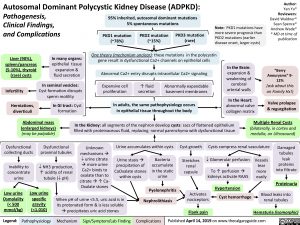
Autosomal Dominant Polycystic Kidney Disease (ADPKD):
Pathogenesis,
Clinical Findings,
and Complications
Author:
Yan Yu*
Reviewers:
David Waldner*
Sean Spence*
Andrew Wade*
* MD at time of
publication
Legend: Published April 14, 2019 on www.Pathophysiology Mechanism Sign/Symptom/Lab Finding Complications thecalgaryguide.com
One theory (mechanism unclear): these mutations in the polycystin
gene result in dysfunctional Ca2+ channels on epithelial cells
PKD1 mutation
(~78%)
Abnormal Ca2+ entry disrupts intracellular Ca2+ signaling
In the Kidney: all segments of the nephron develop cysts: sacs of flattened epithelium
filled with proteinaceous fluid, replacing normal parenchyma with dysfunctional tissue
PKD2 mutation
(~15%)
Expansive cell
proliferation
Low urine
Osmolality
(< 500
mmol/kg)
Abnormally expandable
basement membranes
PKD3 mutation
(rare)
↑ fluid
secretion
95% inherited, autosomal dominant mutations
5% spontaneous mutations
In adults, the same pathophysiology occurs
in epithelial tissue throughout the body
When pH of urine <5.5, uric acid is in
its protonated form & is less soluble
àprecipitates uric acid stones
Nephrolithiasis
Urine accumulates within cysts Cyst growth
Pyelonephritis
Damaged
tubules
leak
proteins
into filtrate
Proteinuria
Flank pain
Inability to
concentrate
urine
Low urine
specific
gravity
(<1.010)
¯ NH3 production,
↑ acidity of renal
tubule (¯ pH)
Activates
nociceptors Cyst hemorrhage
Urine stasis à
precipitation of
CaOxalate stones
within cysts
Multiple Renal Cysts
(bilaterally, in cortex and
medulla, on Ultrasound)
In the Brain:
expansion &
weakening of
cerebral
arterial walls
“Berry
Aneurysms” 9-
12%
(ask about this
on Family Hx!)
In many organs:
epithelial tissue
expansion &
fluid secretion
In the Heart:
abnormal valve
collagen matrix
Valve prolapse
& regurgitation
Liver (90%),
spleen/pancreas
(5-10%), thyroid
(rare) cysts
In seminal vesicles:
Cyst formation disrupts
sperm motility
Infertility
In GI tract: Cyst
formation
Herniations,
diverticuli
Dysfunctional
collecting ducts
Abdominal mass
(enlarged kidneys)
(may be palpable)
Blood leaks into
renal tubules
Hematuria (isomorphic)
Bacteria
accumulate
in the static
urine
Dysfunctional
proximal tubules
Unknown
mechanisms à
¯ urine citrate
àmore urine
Ca2+ binds to
oxalate than to
citrate à↑ Ca-
Oxalate stones
Note: PKD1 mutations have
more severe prognosis than
PKD2 mutations (earlier
disease onset, larger cysts)
Vessels
tear
more
easily
Stretches
renal
capsule
Cysts compress renal vasculature
¯ Glomerular perfusion
To ↑ perfusion à
kidneys activate RAAS
Hypertension
Foundations
Systems
Other Languages
Nephrology Kidney Injury Autosomal Dominant Polycystic Kidney Disease (ADPKD) autosomal-dominant-polycystic-kidney-disease-adpkd