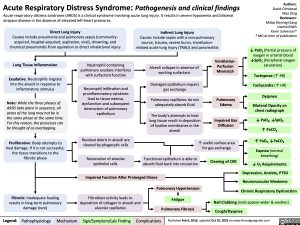
Acute Respiratory Distress Syndrome: Pathogenesis and clinical findings Acute respiratory distress syndrome (ARDS) is a clinical syndrome involving acute lung injury. It results in severe hypoxemia and bilateral
Authors: David Olmstead Mao Ding Reviewers: Midas (Kening) Kang Usama Malik Kevin Solverson* * MD at time of publication
↓ PaO2 (Partial pressure of oxygen in arterial blood ↓SpO2 (Peripheral oxygen saturation)
Tachypnea (↑ RR) Tachycardia (↑ HR)
Dyspnea
Bilateral Opacity on chest radiograph
↓ PaO2, ↓SpO2
↑ PaCO 2
↑ PaO2, ↓PaCO2 Eupnea (normal
breathing)
↓ O2 Requirements Depression, Anxiety, PTSD Neuromuscular Weakness
Chronic Respiratory Dysfunction
airspace disease in the absence of elevated left-heart pressures.
Direct Lung Injury
Causes include pneumonia and pulmonary sepsis (community- acquired, hospital-acquired, aspiration, viral), drowning, and chemical pneumonitis from aspiration or direct inhalational injury
Indirect Lung Injury
Causes include sepsis with a non-pulmonary source, trauma, severe burns, transfusion- related acute lung injury (TRALI) and pancreatitis
Lung Tissue Inflammation
Exudative: Neutrophils migrate into the alveoli in response to inflammatory stimulus
Note: While the three phases of ARDS take place in sequence, all areas of the lung may not be in the same phase at the same time. For this reason, the processes can be thought of as overlapping.
Proliferative: Body attempts to heal damage. If it is not successful, the tissue transitions to the fibrotic phase
Neutrophil-containing pulmonary exudate interferes with surfactant function
Neutrophil infiltration and proinflammatory cytokines lead to tissue edema, dysfunction and subsequent destruction of pulmonary epithelium
Residual debris in alveoli are cleared by phagocytic cells
Restoration of alveolar epithelial cells.
Alveoli collapse in absence of working surfactant
Damaged epithelium impairs gas exchange
Pulmonary capillaries do not adequately absorb fluid
The body’s attempts to heal lung tissue result in deposition of hyaline membranes in the alveoli
Ventilation- Perfusion Mismatch
Pulmonary Edema
Impaired Gas Diffusion
Functional epithelium is able to absorb fluid back into circulation
↑ useful surface area for gas exchange
Clearing of CXR
Impaired Function After Prolonged Illness
Pulmonary Hypertension
Fibrotic: Inadequate healing results in long-term pulmonary damage (rare)
Fibroblast activity leads to deposition of collagen in alveoli and alveolar capillaries
Fatigue Pulmonary Fibrosis
Nail Clubbing (nails appear wider & swollen) Cough/Dyspnea
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published Feb 6, 2018, updated Oct 10, 2023 on www.thecalgaryguide.com
Acute Respiratory Distress Syndrome: Note: Acute respiratory distress syndrome is a clinical
Authors: David Olmstead Reviewers: Midas (Kening) Kang Usama Malik Kevin Solverson* * MD at time of publication
Pathogenesis and clinical findings
Direct Lung Injury
Causes include pneumonia and pulmonary sepsis (community-acquired, hospital-acquired, aspiration, viral), drowning, and chemical pneumonitis from aspiration or direct inhalational injury
Indirect Lung Injury
syndrome involving acute lung injury. It results in severe hypoxemia and bilateral airspace disease in the absence of elevated left-heart pressures.
Causes include sepsis with a non-pulmonary source, trauma, severe burns, transfusion-related acute lung injury (TRALI) and pancreatitis
Lung Tissue Inflammation
Exudative: Neutrophils migrate into the alveoli in response to inflammatory stimulus
Note: While the three phases of ARDS take place in sequence, all areas of the lung may not be in the same phase at the same time. For this reason, the processes can be thought of as overlapping.
Proliferative: Body attempts to heal damage. If it is not successful, the tissue transitions to the fibrotic phase
Neutrophil-containing pulmonary exudate interferes with surfactant function
Neutrophil infiltration and proinflammatory cytokines lead to tissue edema, dysfunction and subsequent destruction of pulmonary epithelium
Abbreviations:
PaO2: Partial pressure of oxygen in arterial blood
SpO2: Peripheral oxygen saturation.
CXR: Chest radiograph.
Residual debris in alveoli are cleared by phagocytic cells
Restoration of alveolar epithelial cells.
Alveoli collapse in absence of working surfactant
Damaged epithelium impairs gas exchange
Pulmonary capillaries do not adequately absorb fluid
The body’s attempts to heal lung tissue result in
deposition of hyaline membranes in the alveoli
Ventilation- Perfusion Mismatch
Pulmonary Edema
Impaired Gas Diffusion
↓ PaO2, ↓SpO2 Tachypnea
Tachycardia
Dyspnea
Bilateral Opacity on CXR
↓ PaO , ↓SpO 2 2
↑ PaCO2
↑ PaO2, ↓PaCO2 Eupnea
↓ O2 Requirements
Clearing of CXR
Depression, Anxiety, PTSD
Neuromuscular Weakness
Chronic Respiratory Dysfunction
↑ useful surface area for gas exchange
Functional epithelium is able to absorb fluid back into circulation
Impaired Function After Prolonged Illness
Fibrotic: Inadequate healing results in long-term pulmonary damage (rare)
Fibroblast activity leads to deposition of collagen in alveoli and alveolar capillaries
Pulmonary Fibrosis
Pulmonary Hypertension
Cough/Dyspnea Nail Clubbing Fatigue
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published February 06, 2018 on www.thecalgaryguide.com