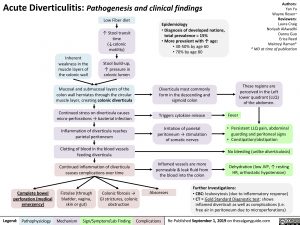
Acute Diverticulitis: Pathogenesis and clinical findings
Authors: Yan Yu Wayne Rosen* Reviewers: Laura Craig Noriyah AlAwadhi Danny Guo Erica Reed Maitreyi Raman* * MD at time of publication
These regions are perceived in the Left lower quadrant (LLQ) of the abdomen.
• PersistentLLQpain,abdominal guarding and peritoneal signs
• Constipation/obstipation
No bleeding (unlike diverticulosis)
Dehydration (low JVP, ↑ resting HR, orthostatic hypotension)
Inherent weakness in the muscle layers of the colonic wall
Low Fiber diet
↑ Stool transit time (↓colonic motility)
Stool build-up, ↑ pressure in colonic lumen
Epidemiology
• Diagnosis of developed nations,
total prevalence = 15%
• More prevalent with ↑ age:
• 30-50% by age 60 • 70% by age 80
Diverticula most commonly form in the descending and sigmoid colon
Triggers cytokine release
Irritationofparietal peritoneum → stimulation ofsomaticnerves
Inflamed vessels are more permeable & leak fluid from the blood into the colon
Mucosal and submucosal layers of the colon wall herniates through the circular muscle layer, creating colonic diverticula
Continued stress on diverticula causes micro-perforations → bacterial infection
Inflammation of diverticula reaches parietal peritoneum
Clotting of blood in the blood vessels feeding diverticula
Continued inflammation of diverticula causes complications over time
Fever
Complete bowel perforation (medical emergency)
Fistulae (through bladder, vagina, skin or gut)
Colonic fibrosis → GI strictures, colonic obstruction
Abscesses
Further Investigations:
• CBC: leukocytosis (due to inflammatory response) • CT = Gold Standard Diagnostic test: shows
inflamed diverticuli as well as complications (i.e. free air in peritoneum due to microperforations)
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Re-Published September 1, 2019 on thecalgaryguide.com