The Alveolar-arterial pO2 gradient:
Author: Yan Yu Reviewers: Steven Liu, Amogh K. Agrawal, Ciara Hanly, Xiumei Deng (邓秀梅), Zesheng Ye (叶泽生), Yonglin Mai (麦泳琳)*, Juri Janovcik* * MD at time of publication
Why it exists, and why we care
Key Abbreviations:
• pO2: partial pressure of O2,
aka. “O2 content”.
• PaO2: partial pressure of O2 in
the arteries. Measured directly
via Arterial Blood Gas (ABGs). • PAO2: partial pressure of O2 in
the Alveoli. (Can’t be measured directly, must be calculated).
Theoretically, in lung capillaries adjacent to alveoli: O2
should diffuse from alveoli into lung capillaries, and no O2 should be lost from the blood until the blood reaches the systemic arteries – so the PaO2 should equal PAO2.
But in reality…
Blood in the lung capillaries are not fully oxygenated to begin with:
Since gravity causes more blood to settle to the lung bases, there is too much blood there for it all to be fully oxygenated by the alveoli.
Less well-oxygenated blood from lung bases reduces the blood’s overall pO2
Less oxygenated blood from systemic veins are mixed into oxygenated blood from the lungs (“Venous admixture”):
Venous drainage from the bronchial artery directly mixes with the pulmonary veins (oxygenated blood)
Some veins in the coronary circulation drain into the left ventricle, instead of into the coronary sinus/R atrium
Thus, O2 content of blood when it finally reaches the systemic arteries (PaO2) is less than the O2 content in the alveoli (PAO2)
PAO2 – PaO2 = the pO2 “gradient” between the alveoli and the systemic arteries
Note: Abnormally high A- a gradients indicate issues with gas diffusion between alveoli & the pulmonary capillaries.
Note: some respiratory pathologies can present with a normal A-a gradient as well (see relevant slides)
Normal A-a Gradient: <15 mmHg
High A-a Gradient (>15 mmHg) is always a sign of pathology (see relevant slides)
Legend:
Definitions
Explanations
Sign/Symptom/Lab Finding
Complications
Published September 4, 2013, updated October 5, 2021 on www.thecalgaryguide.com
The Alveolar-arterial pO2 gradient: Explainingtheformula A-aGradient=PO –PO
(The simplified explanation)
A 2
a
2
For an explanation of the physiology behind
why an A-a gradient exists, please consult: “The Alveolar-arterial pO2 gradient: Why it exists, and why we care”
Fraction of inhaled air made up of O2 (21%, if atmospheric)
Partial Pressure of O2 within the alveoli:
Partial Pressure of O2 in systemic arteries Measured directly via Arterial Blood Gas (ABG)
PAO2 =
(Total pressure of O2 inhaled into alveoli)
(Air pressure generated by CO2 – molecules that are produced by
the consumption of O2 molecules
PAO2 = FiO2(PB – PH2O) – (PaCO2/0.8)
Barometric Pressure Total air pressure inhaled into lungs (760mmHg at sea level, and less at higher altitudes)
Partial pressure of water (47 mmHg): Inspired air is humidified once inside airways. Water vapor adds to total inhaled air pressure, and must be accounted for
Partial pressure of dissolved CO2 in arteries, directly measured by an ABG
Respiratory quotient: conversion ratio reflecting how, for every 5 molecules of O2 the blood absorbs or consumes, it releases approximately 4 CO2 molecules into the alveoli
Partial pressure of gaseous CO2 in alveoli (PACO2)
CO2 produced by body metabolism, exhaled into alveoli
Author: Yan Yu Reviewers: Steven Liu, Amogh K. Agrawal, Ciara Hanly, Xiumei Deng (邓秀梅), Zesheng Ye (叶泽生), Yonglin Mai (麦泳琳)*, Juri Janovcik* * MD at time of publication
Legend:
Definitions
Explanations
Sign/Symptom/Lab Finding
Complications
Published September 4, 2013, updated October 5, 2021 on www.thecalgaryguide.com
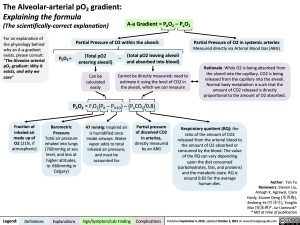
The Alveolar-arterial pO2 gradient:
Explaining the formula
(The scientifically-correct explanation)
For an explanation of the physiology behind
why an A-a gradient exists, please consult: “The Alveolar-arterial pO2 gradient: Why it exists, and why we care”
A-a Gradient = PAO2 – PaO2 Partial Pressure of O2 within the alveoli:
Partial Pressure of O2 in systemic arteries
Measured directly via Arterial Blood Gas (ABG)
Rationale: While O2 is being absorbed from the alveoli into the capillary, CO2 is being released from the capillary into the alveoli. Normal body metabolism is such that the amount of CO2 released is directly proportional to the amount of O2 absorbed.
PAO2 =
(Total pO2 entering alveoli)
Can be calculated easily
– (total pO2 leaving alveoli and absorbed into blood)
Cannot be directly measured; need to estimate it using the level of CO2 in the alveoli, which we can measure
PAO2 = FiO2(PB – PH2O) – (PaCO2/0.8)
Fraction of inhaled air made up of O2 (21%, if atmospheric)
Barometric Pressure Total air pressure inhaled into lungs (760mmHg at sea level, and less at higher altitudes, ie: 660mmHg in Calgary)
47 mmHg: Inspired air is humidified once inside airways. Water vapor adds to total inhaled air pressure, and must be accounted for
Partial pressure of dissolved CO2 in arteries, directly measured by an ABG
Respiratory quotient (RQ): the ratio of the amount of CO2
released from the arterial blood to
the amount of O2 absorbed or
consumed by the blood. The value
of the RQ can vary depending
upon the diet consumed
Note: The respiratory quotient (carbohydrates, fats, and proteins)
(RQ) is always <1 because
and the metabolic state. RQ is
around 0.82 for the average human diet.
Author: Yan Yu Reviewers: Steven Liu, Amogh K. Agrawal, Ciara Hanly, Xiumei Deng (邓秀梅), Zesheng Ye (叶泽生), Yonglin Mai (麦泳琳)*, Juri Janovcik* * MD at time of publication
Legend:
Definitions
Explanations
Sign/Symptom/Lab Finding
Complications
Published September 4, 2013, updated October 5, 2021 on www.thecalgaryguide.com