Yu, Yan – DM I and II pathogenesis – Ready for Faculty.pptx
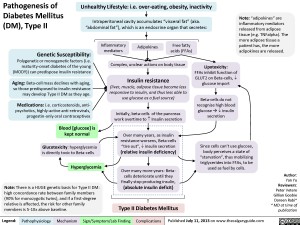
Over many years, as insulin resistance worsens, Beta-cells “tire out”, ? insulin secretion(relative insulin deficiency) Legend:Published July 11, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsAuthor: Yan YuReviewers:Peter VetereGillian GoobieDoreen Rabi** MD at time of publicationBlood [glucose] is kept normalInsulin resistance(liver, muscle, adipose tissue become less responsive to insulin, and thus less able to use glucose as a fuel source)Initially, beta-cells of the pancreas work overtime to ? Insulin secretionPathogenesis of Diabetes Mellitus (DM), Type IIAdipokinesInflammatory mediatorsUnhealthy Lifestyle: i.e. over-eating, obesity, inactivityFree fatty acids (FFAs)Genetic Susceptibility:Polygenetic or monogenetic factors (i.e. maturity-onset diabetes of the young (MODY)) can predispose insulin resistanceMedications: i.e. corticosteroids, anti-psychotics, highly-active anti-retrovirals, progestin-only oral contraceptivesIntraperitoneal cavity accumulates “visceral fat” (aka. “abdominal fat”), which is an endocrine organ that secretes: HyperglycemiaComplex, unclear actions on body tissueSince cells can’t use glucose, body perceives a state of “starvation”, thus mobilizing triglycerides into FFAs, to be used as fuel by cells.Glucotoxicity: hyperglycemia is directly toxic to Beta-cellsOver many more years: Beta-cells deteriorate until they finally stop producing insulin, (absolute insulin deficit)Type II Diabetes MellitusNote: “adipokines” are inflammatory mediators released from adipose tissue (e.g. TNFalpha). The more adipose tissue a patient has, the more adipokines are released.Note: There is a HUGE genetic basis for Type II DM: high concordance rate between family members (90% for monozygotic twins), and if a first-degree relative is affected, the risk for other family members is 5-10x above baseline.Lipotoxicity:FFAs inhibit function of GLUT2 on Beta-cells, ? glucose importBeta-cells do not recognize high blood glucose ? ? insulin secretionAging: Beta-cell mass declines with aging, so those predisposed to insulin resistance may develop Type II DM as they age.
Directly destroy or damage Beta cells, enough to expose its antigens to body’s immune systemForeign antigens structurally mimic Beta-cell antigens (molecular mimicry) immune system attacks both these foreign -and self-antigensLegend:Published July 11, 2013 on www.thecalgaryguide.comMechanismPathophysiologySign/Symptom/Lab FindingComplicationsPathogenesis of Diabetes Mellitus (DM), Type IAuthor: Yan YuReviewers:Peter VetereGillian Goobie*Doreen Rabi* MD at time of publicationGenetic Susceptibility?IDDM1 (HLA) mutations?IDDM2 (Insulin gene) mutationsMutations in the HLA (MHC) gene can either facilitate (or prevent) T-cell receptor binding to Beta-cellsBreakdown of immune system’s self-tolerance of pancreatic Beta-CellsFailure of maturing T-cells in the thymus to develop recognition of the insulin gene ? abnormal attack of insulin producing Beta-cellsType 1 Diabetes MellitusPrimary absolute insulin deficitEnvironmental TriggersAuto-immune attack on beta cells(involves both the innate and acquired immune systems: monocytic pancreatic islet infiltration, and the direct T-cell attack of Beta cells known as “insulitis”)Blunted insulin response to IV glucose”Pre-diabetes”Auto-antibodies produced against Beta cellsAnti-Insulin and anti-GAD65 detectable in serumNote: Number of auto-antibodies detected predicts likelihood of developing DM Diet (cow’s milk, nitrosamines)Viruses (Rubella, Coxsakie, Mumps)Stresses (repeated sicknesses, surgery, puberty)Drugs/Toxins (vacor, alloxa, streptozocin, pentamidine)Loss of Beta-cell mass to less than half of original massHigh post-prandial [glucose]Still asymptomaticOver time, only <10% of original Beta cells are still functional
103 kB / 465 words
Foundations
Systems
Other Languages
Endocrinology Diabetes Mellitus: pathogenesis and clinical findings Pathogenesis of Diabetes Mellitus (DM), Type II Pathogenesis of Diabetes mellitus DM), Type II