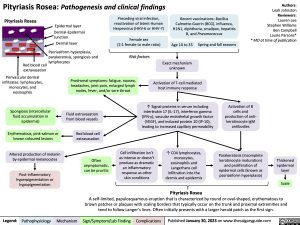
Pityriasis Rosea: Pathogenesis and clinical findings
Authors: Leah Johnston Reviewers: Lauren Lee Stephen Williams Ben Campbell Laurie Parsons* * MD at time of publication
Pityriasis Rosea
Epidermal layer
Dermal-Epidermal Junction
Dermal layer
Psoriasiform hyperplasia, parakeratosis, spongiosis and
Preceding viral infection, reactivation of latent Human Herpesvirus (HHV-6 or HHV-7)
Female sex
(2:1 female to male ratio)
Risk factors
Recent vaccinations: Bacillus Calmette-Guerin (BCG), influenza, H1N1, diphtheria, smallpox, hepatitis B, and Pneumococcus
Red blood cell lymphocytes extravasation
Perivascular dermal infiltrates: lymphocytes, monocytes, and eosinophils
Spongiosis (intercellular fluid accumulation in epidermis)
Erythematous, pink-salmon or brown coloured lesions
Altered production of melanin by epidermal melanocytes
Post-inflammatory hyperpigmentation or hypopigmentation
Prodromal symptoms: fatigue, nausea, headaches, joint pain, enlarged lymph nodes, fever, and/or sore throat
Age 10 to 35
Exact mechanism unknown
Activation of T-cell mediated host immune response
↑ Signal proteins in serum including interleukin 17 (IL-17), interferon gamma (IFN-γ), vascular endothelial growth factor (VEGF), and induced protein 10 (IP-10), leading to increased capillary permeability
Spring and fall seasons
Fluid extravasation from blood vessels
Red blood cell extravasation
Often asymptomatic, can be pruritic
Cell infiltration isn’t as intense or doesn’t produce as dramatic an inflammatory response as other skin conditions
↑ CD4 lymphocytes, monocytes, eosinophils and Langerhans cell infiltration into the dermis and epidermis
Pityriasis Rosea
Activation of B cells and production of anti- keratinocyte IgM antibodies
Parakeratosis (incomplete keratinocyte maturation) and proliferation of epidermal cells (known as psoriasiform hyperplasia)
Thickened epidermal layer
Scale
A self-limited, papulosquamous eruption that is characterized by round or oval-shaped, erythematous to brown patches or plaques with scaling borders that typically occur on the trunk and proximal extremities and tend to follow Langer’s lines. Often initially presents with a larger herald patch as the first sign.
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
Complications
Published January 30, 2023 on www.thecalgaryguide.com