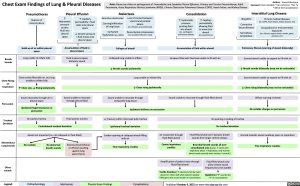
Chest Exam Findings of Lung & Pleural Diseases
Note: Please see slides on pathogenesis of Transudative and Exudative Pleural Effusions, Primary and Tension Pneumothorax, Adult Pneumonia, Acute Respiratory Distress Syndrome (ARDS), Chronic Obstructive Pulmonary Disease (COPD), Heart Failure, and Kidney Disease
Authors: Sravya Kakumanu Reviewers: Ben Campbell, *Tara Lohmann, *Yan Yu * MD at time of publication
Interstitial Lung Disease
Pneumothorax
Rupture of visceral pleura
Build-up of air within pleural space
Pleural Effusion
Atelectasis
Consolidation
↑ Hydrostatic pressure pushes fluid into pleural space
↑ Capillary permeability = fluid leaks into pleural space
↓ Oncotic pressure = fluid moves into pleural space
Bronchus obstructed
Scarring/infiltration of lung tissue
Surfactant dysfunction (ex. ARDS)
Loss of contact between visceral and parietal pleura
(ex. effusion, pneumothorax)
Parenchymal compression (ex. loculated effusion, mass)
↑ Hydrostatic
pressure
pushing fluid
into alveoli (ex. cardiogenic pulmonary edema)
↑ Capillary
permeability
allowing fluid
to move into
alveoli (ex. pneumonia)
Idiopathic
Connective tissue diseases
Sarcoidosis, Amyloidosis
Chronic medical diseases
(ex. COPD, heart failure, kidney disease, etc)
Occupational or environmental exposures
(ex. silicosis, organic dusts, metals, gases, aerosols, etc)
Accumulation of fluid in pleural space
Collapse of alveoli
Accumulation of fluid within alveoli
Pulmonary fibrosis (scarring of alveoli bilaterally)
Breath Sounds
Lung unable to inflate fully Fluid in pleural space Collapsed lung unable to inflate Airspace filled with fluid and unable to fill with air dampens sound
↓ Breath sounds ipsilaterally
Scarred alveoli unable to expand to fill with air
↓ Breath sounds bilaterally (may not be noticeable)
Chest Rising on Inspiration
Chest cavity filled with air, but lung Lung unable to inflate fully Scarred alveoli unable to expand to fill with air unable to inflate fully
↑ Chest size, ↓ Rising ipsilaterally
↓ Chest rising ipsilaterally ↓ Chest rising bilaterally (may not be noticeable)
Percussion
Sound resonates through air in pleural space
Ipsilateral hyperresonance on percussion
Sound unable to resonate through pleural fluid
Sound unable to resonate through compacted lung tissue
Ipsilateral dullness on percussion
Sound unable to resonate through fluid-filled alveoli
Diffuse scarring of alveoli
No notable changes on percussion
Tracheal Deviation
Air pushes trachea Fluid pushes trachea ↓ Pressure within chest wall pulls trachea No pushing or pulling of trachea
Contralateral tracheal deviation Ipsilateral tracheal deviation No tracheal deviation
Adventitious Lung Sounds
Alveoli not impacted (i.e. not collapsed or fluid-filled)
Sudden opening of collapsed alveoli filling with air
Fine inspiratory crackles
Air movement through fluid-filled alveoli
Coarse inspiratory crackles
Fluid-filled alveoli can’t dampen breath sounds from larger central airways
Bronchial breath sounds all over consolidated area (harsh, ↑ pitch with expiratory phase > inspiratory; only normal when heard centrally over trachea + bronchi)
Scarred inelastic alveoli suddenly open on inspiration
Fine inspiratory crackles
No crackles
No abnormal breath sounds
Severe pneumothorax or effusion pushing against lung parenchyma
Other sounds
Amplification of patient voice through fluid-filled alveoli
Tactile fremitus (↑ vibrations felt by hand placed on chest wall when patient speaks) *Whispers also sound louder on auscultation
Fluid-filled alveoli only allow certain sound frequencies to be audible
Egophony (“E” sounds like “A” on auscultation)
Legend:
Pathophysiology
Mechanism
Physical Exam Findings
Complications
Published October 9, 2022 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Respirology Disorders of the Pleura/Mediastinum/Chest wall Chest Exam Findings of Lung & Pleural Diseases chest-exam-findings-of-lung-pleural-diseases