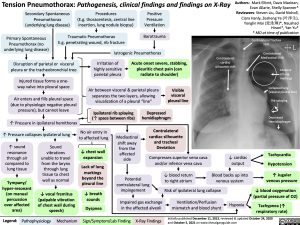
Tension Pneumothorax: Pathogenesis, clinical findings and findings on X-Ray
Authors: Mark Elliott, Davis Maclean, Evan Allarie, Shelly Spanner* Reviewers: Steven Liu, David Nicholl, Ciara Hanly, Zesheng Ye (叶泽生), Yonglin Mai (麦泳琳)*, Naushad Hirani*, Yan Yu* * MD at time of publication
Contralateral Trachea Shift
Contralateral Mediastinal Shift
Absence of lung markings
Collapsed lung (visceral pleural line)
Rib splaying
Depressed Hemidiaphragm
Tachycardia Hypotension
↑ Jugular venous pressure
↓ blood oxygenation (partial pressure of O2)
Tachypnea (↑ respiratory rate)
Secondary Spontaneous Pneumothorax (underlying lung disease)
Procedures
(E.g. thoracentesis, central line insertion, lung nodule biopsy)
Positive Pressure Ventilation
Barotrauma
Primary Spontaneous Pneumothorax (no underlying lung disease)
Traumatic Pneumothorax
E.g. penetrating wound, rib fracture
Iatrogenic Pneumothorax
Disruption of parietal or visceral pleura or the tracheobronchial tree
Injured tissue forms a one- way valve into pleural space
Air enters and fills pleural space (due to physiologic negative pleural pressure), but cannot leave
↑ Pressure in ipsilateral hemithorax ↑ Pressure collapses ipsilateral lung
Irritation of highly sensitive parietal pleura
Acute onset severe, stabbing, pleuritic chest pain (can radiate to shoulder)
Contralateral cardiac silhouette shift
Air between visceral & parietal pleura separates the two layers, allowing visualization of a pleural “line”
Visible visceral pleural line
Ipsilateral rib splaying (↑ space between ribs)
Depressed hemidiaphragm
Contralateral cardiac silhouette
and tracheal Deviation
Compresses superior vena cava and/or inferior vena cava
↑ sound resonance through air compared to lung tissue
Tympany/ hyper-resonant (on manual percussion over affected area)
Sound vibrations unable to travel from the larynx through lung tissue to chest wall as normal
↓ vocal fremitus (palpable vibration of chest wall during speech)
No air entry in to affected lung
↓ chest wall expansion
Lack of lung markings beyond the pleural line
↓ breath sounds
Dyspnea
Mediastinal shift away from the affected side
↓ cardiac output
Blood backs up into venous system
Potential contralateral lung impingement
Impaired gas exchange in the affected alveoli
↓ blood return to right atrium
Risk of ipsilateral lung collapse
Ventilation/Perfusion mismatch and blood shunt
Hypoxia
Legend:
Pathophysiology
Mechanism
Sign/Symptom/Lab Finding
X-Ray Findings
Initially published December 11, 2013, reviewed & updated October 24, 2020 and October 5, 2021 on www.thecalgaryguide.com
Foundations
Systems
Other Languages
Radiology Body Radiology Tension Pneumothorax: Pathogenesis, clinical findings, and findings on X-ray Tension Pneumothorax