SEARCH RESULTS FOR: asthma
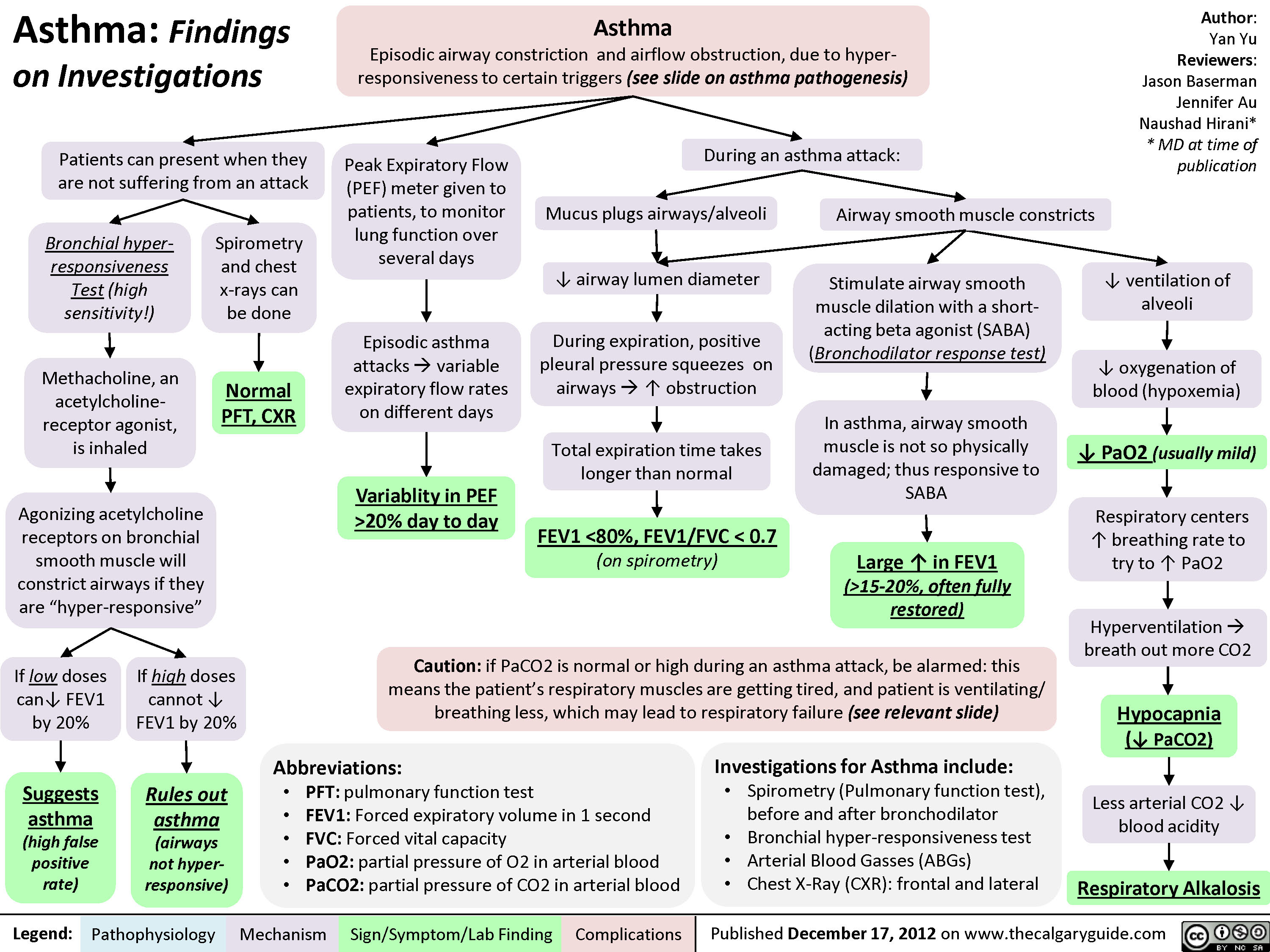
Asthma: Findings on Investigations
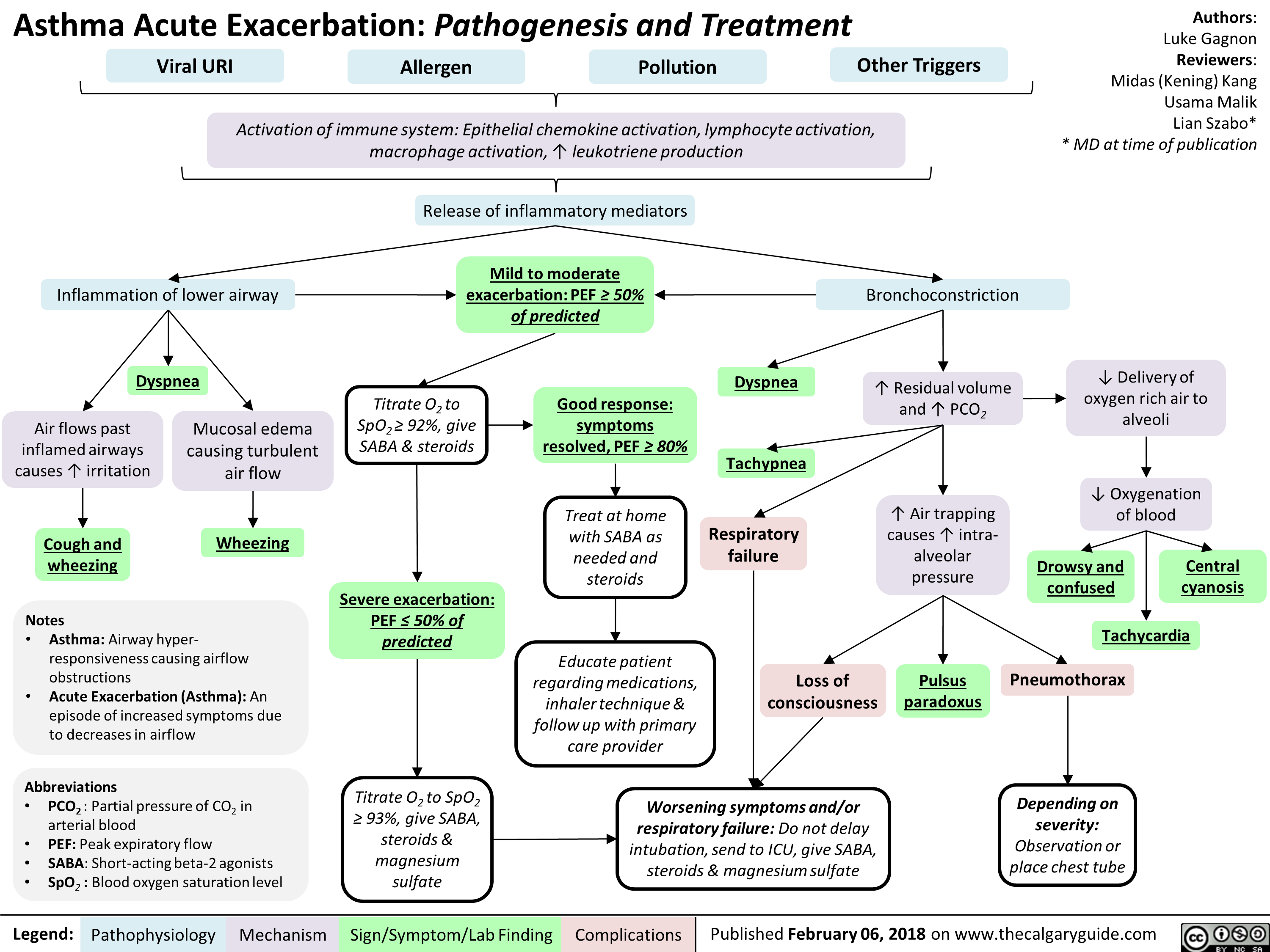
Asthma Acute Exacerbation: Pathogenesis and Treatment
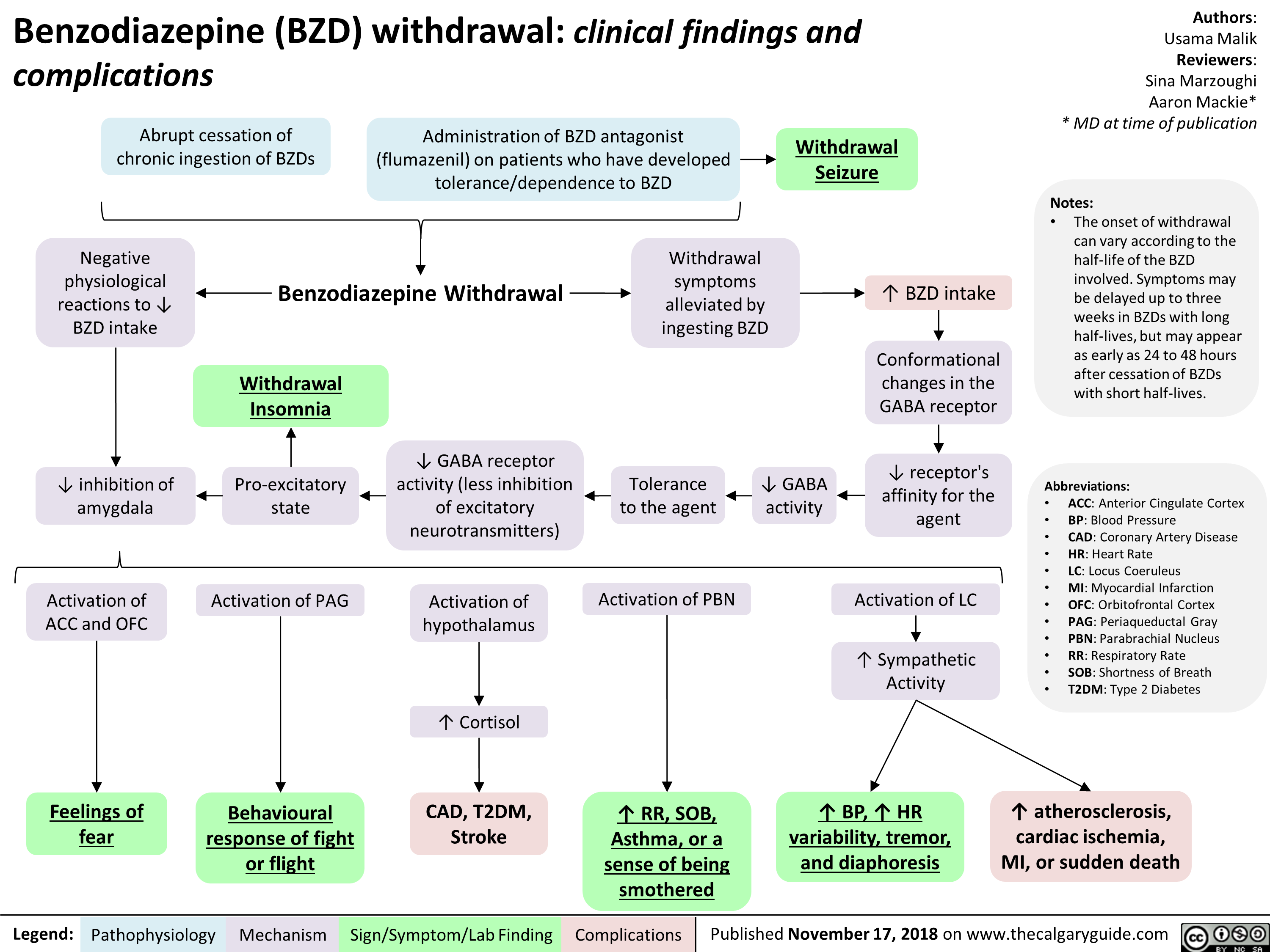
Benzodiazepine (BZD) withdrawal: clinical findings and complications
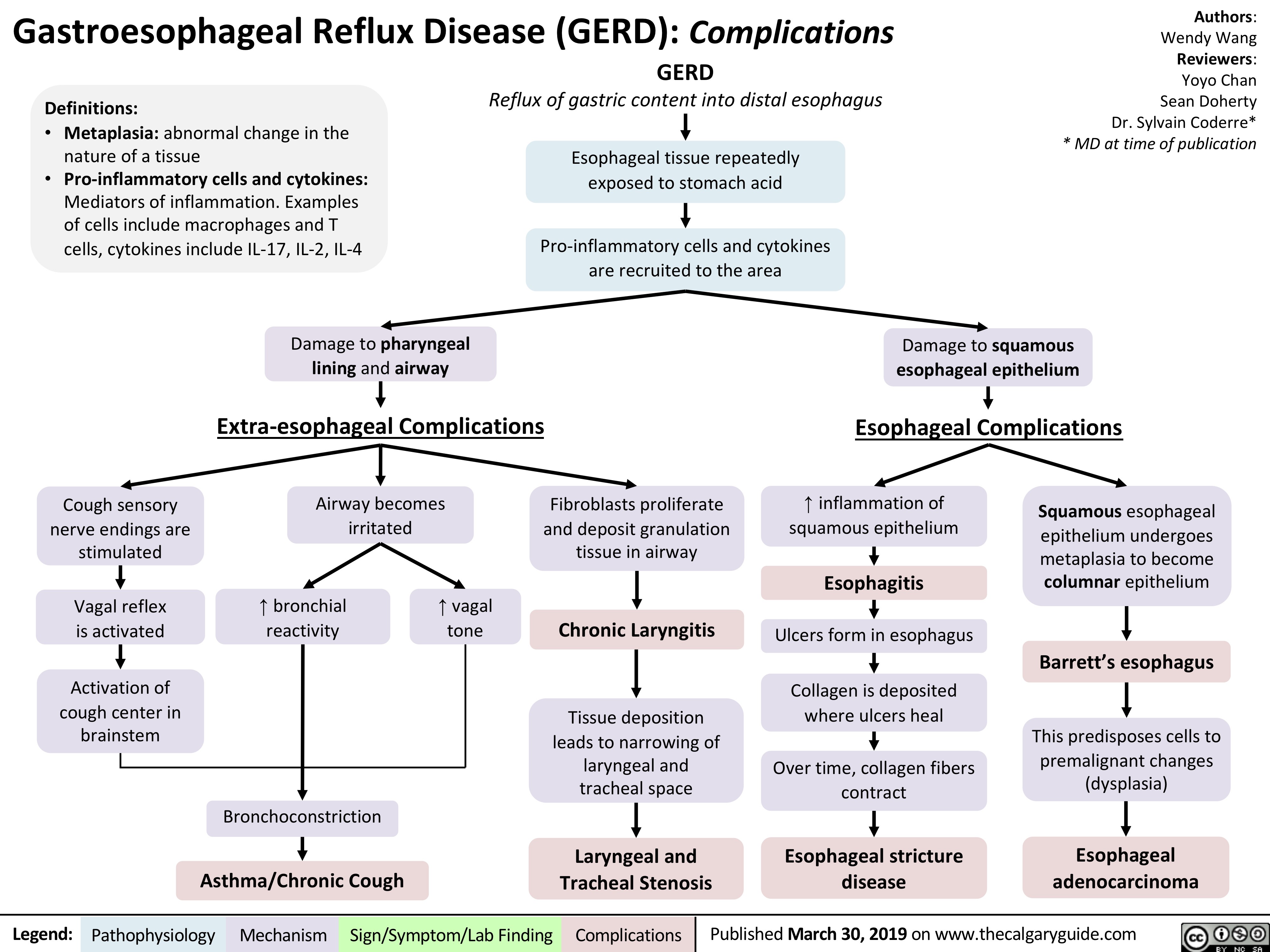
gastroesophageal-reflux-disease-gerd-complications
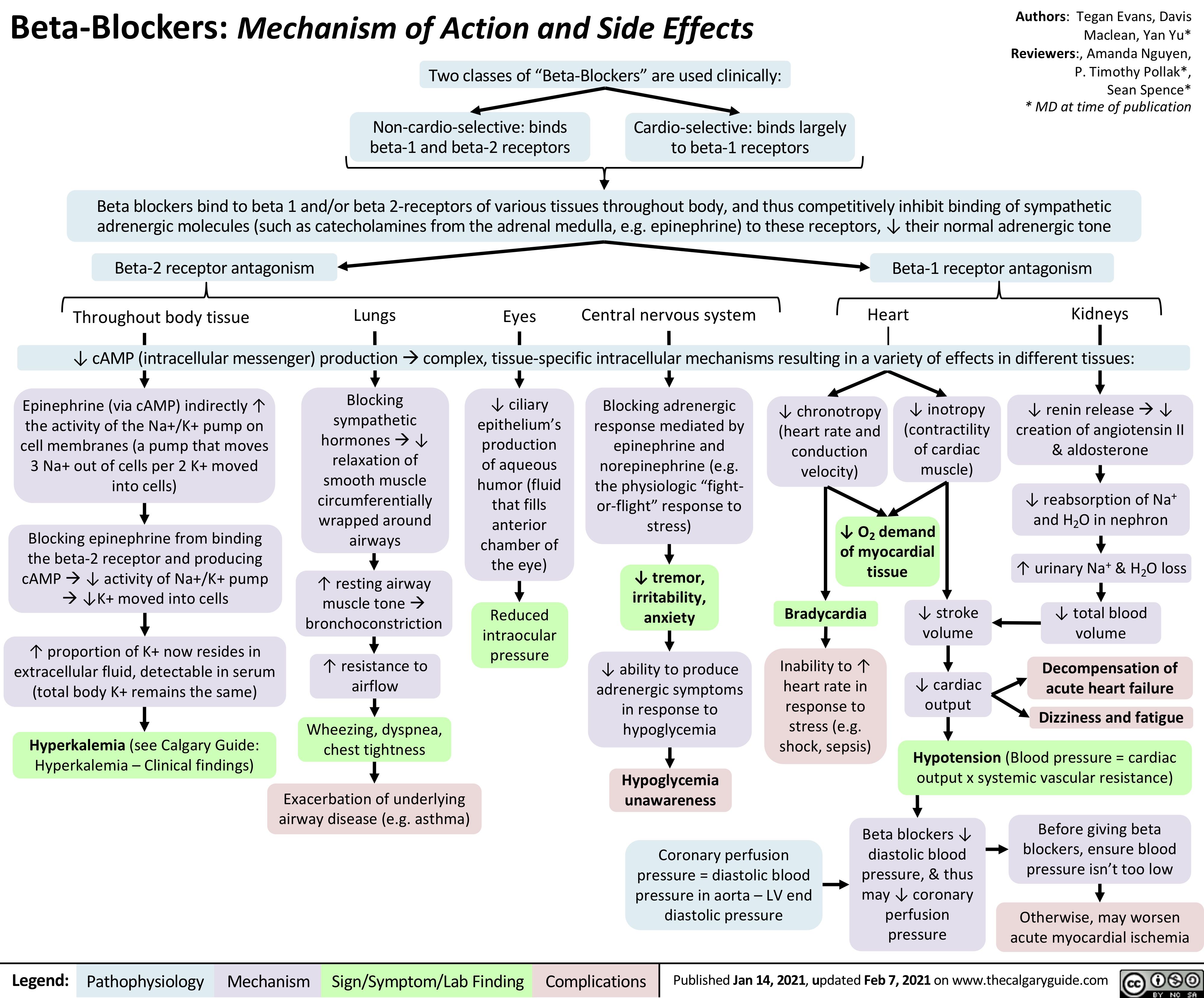
Beta-Blockers-Mechanism-of-Action-and-Side-Effects
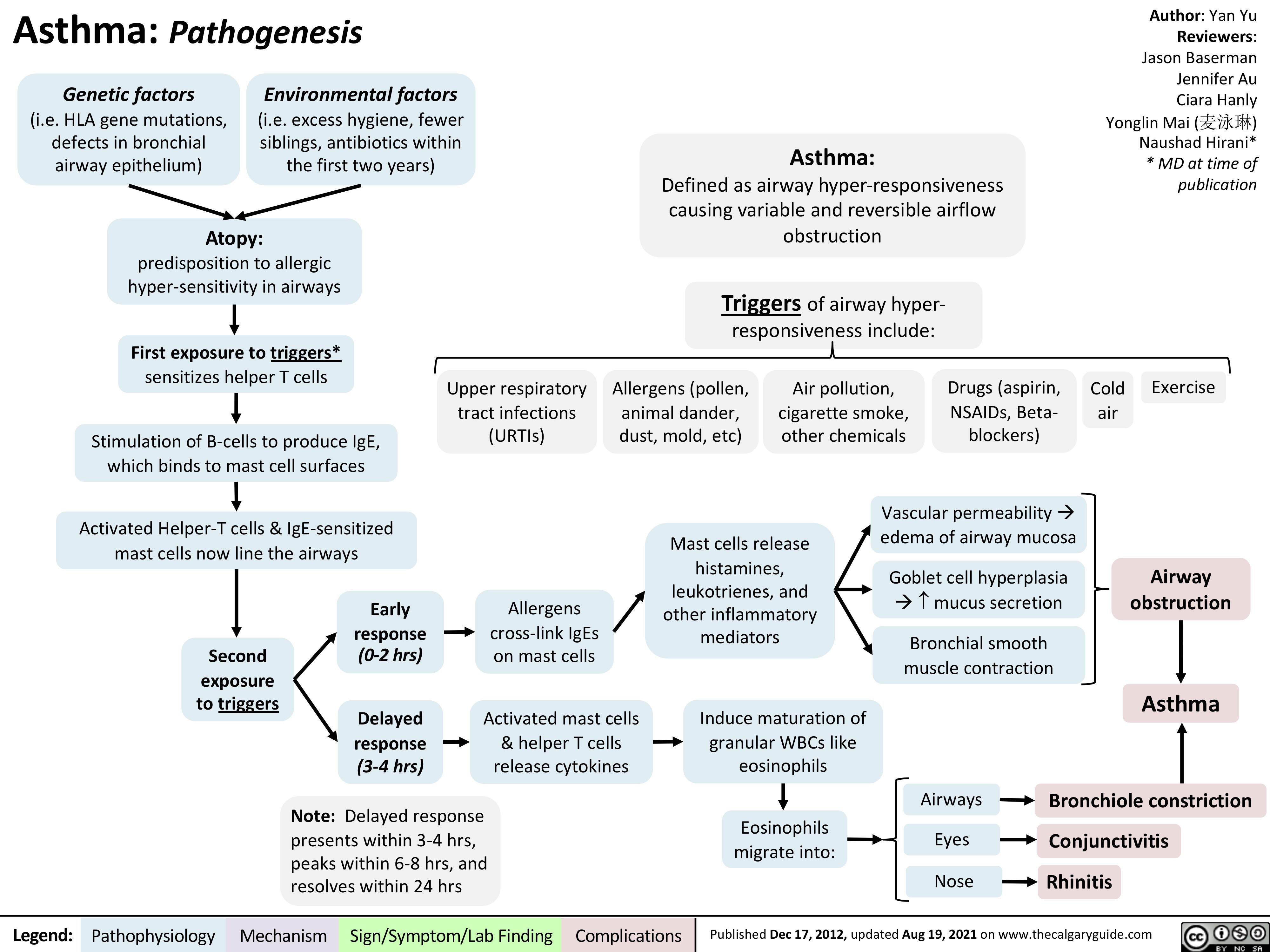
asthma-pathogenesis
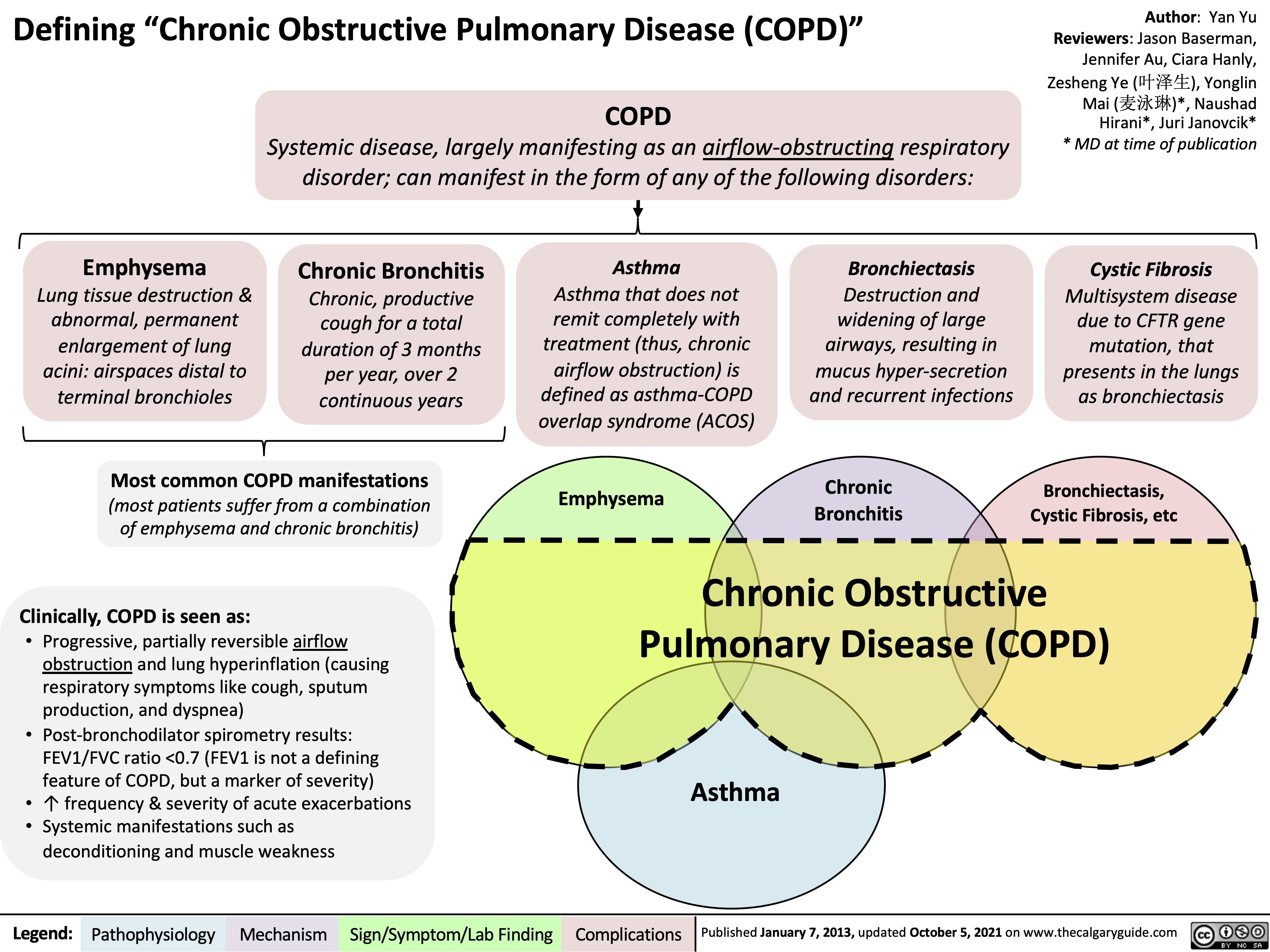
copd-overview-and-definitions
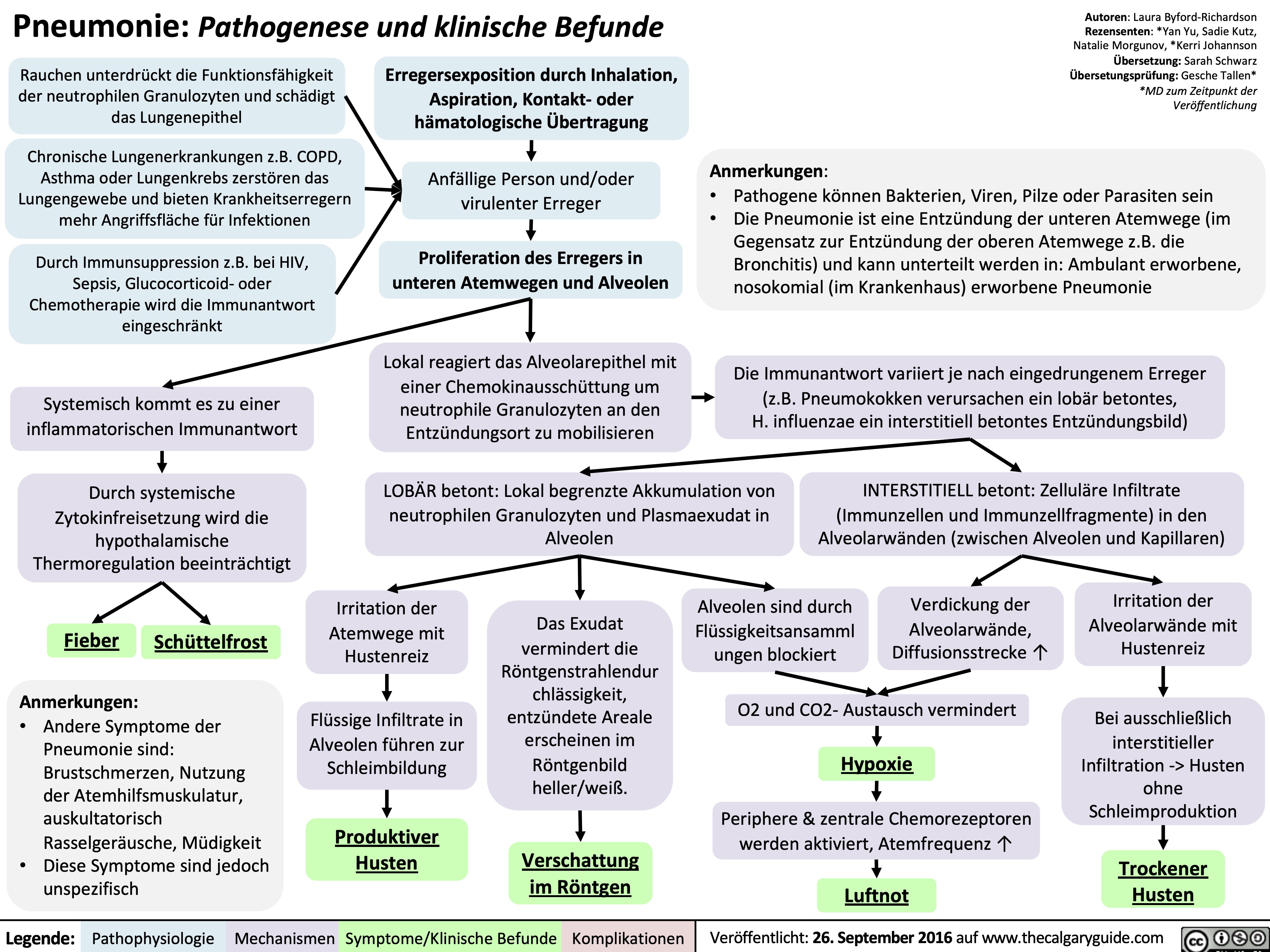
Pneumonie: Pathogenese und klinische Befunde
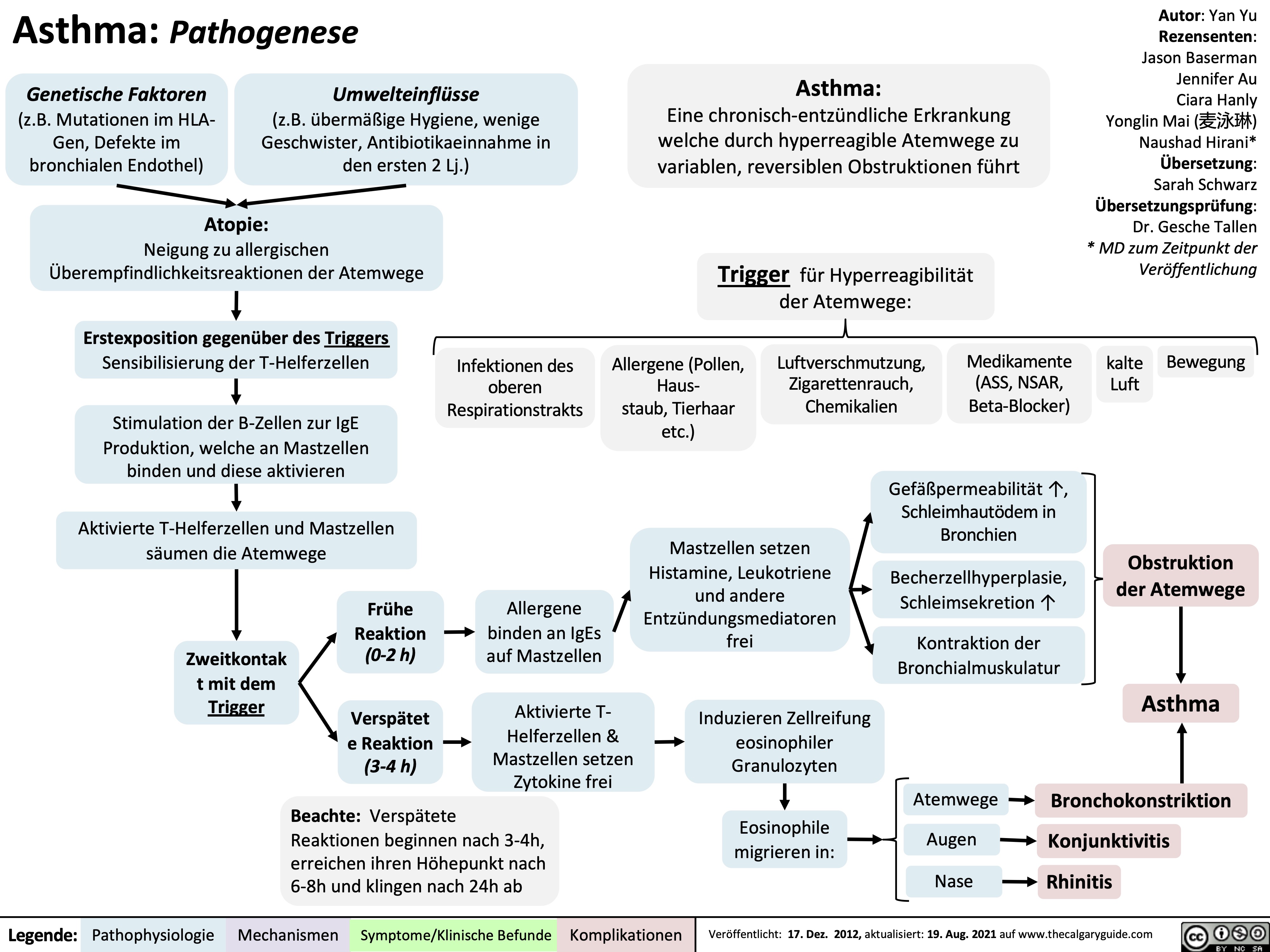
Asthma: Pathogenese
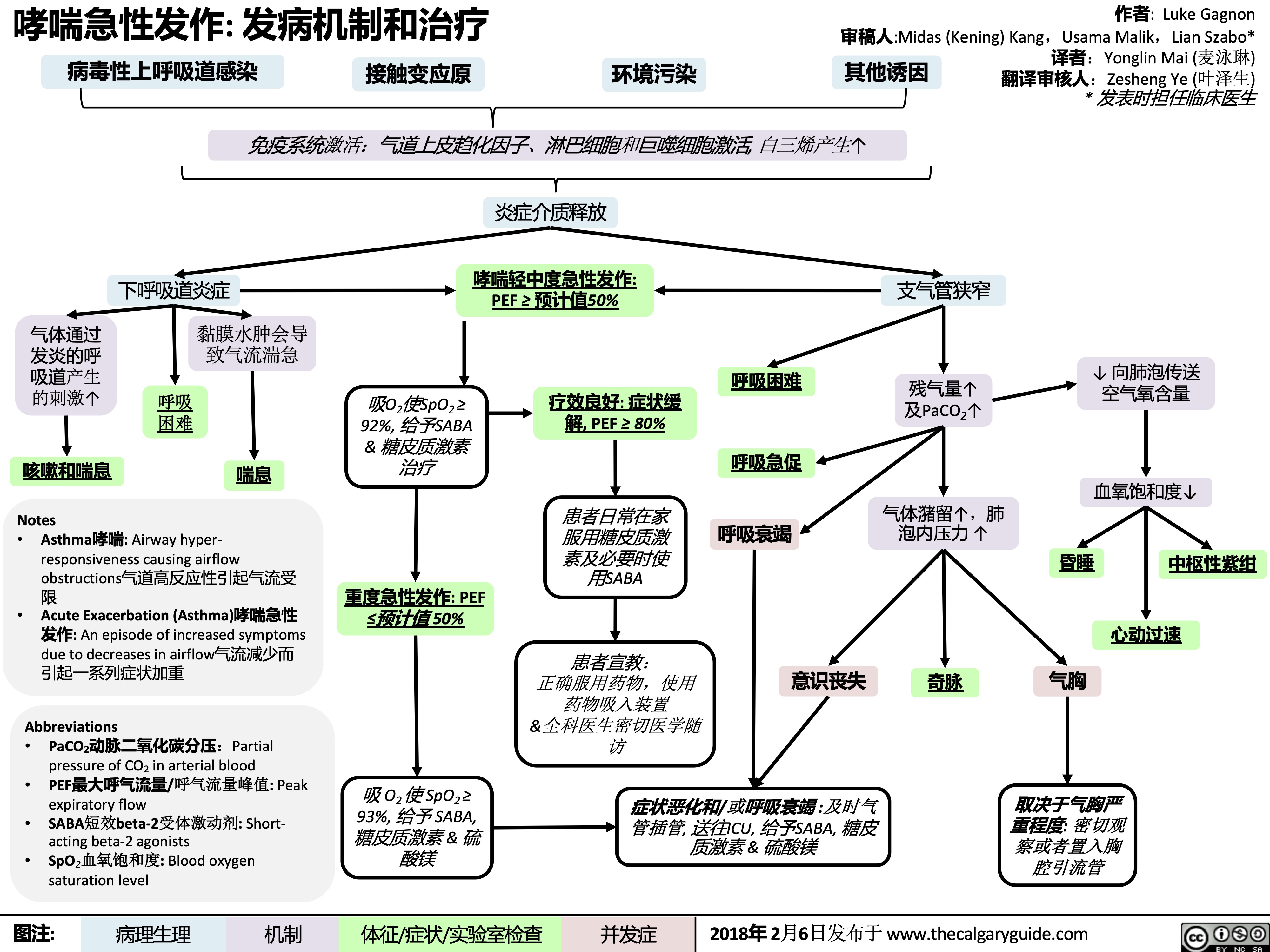
哮喘急性发作-发病机制和治疗
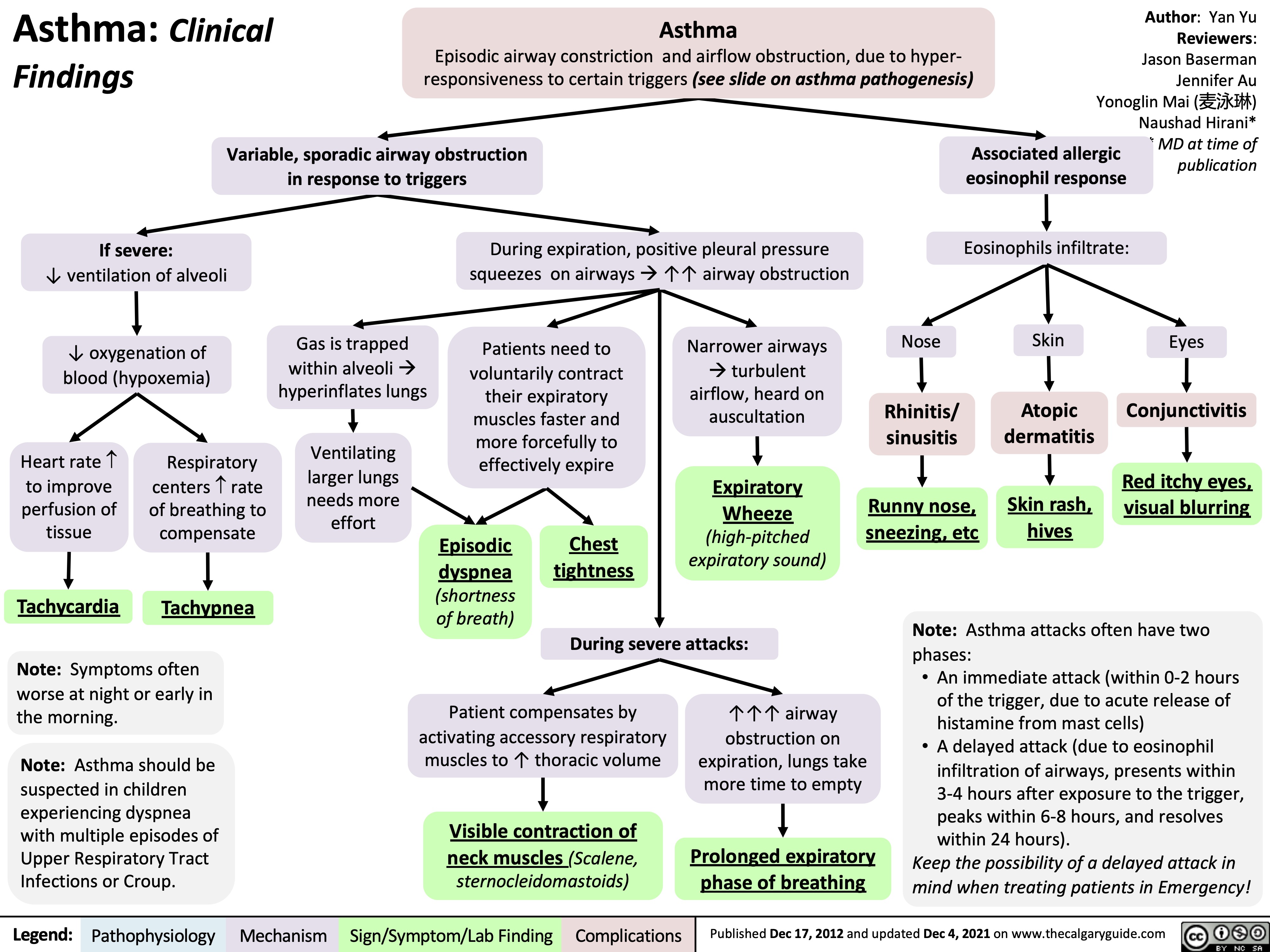
Asthma clinical findings
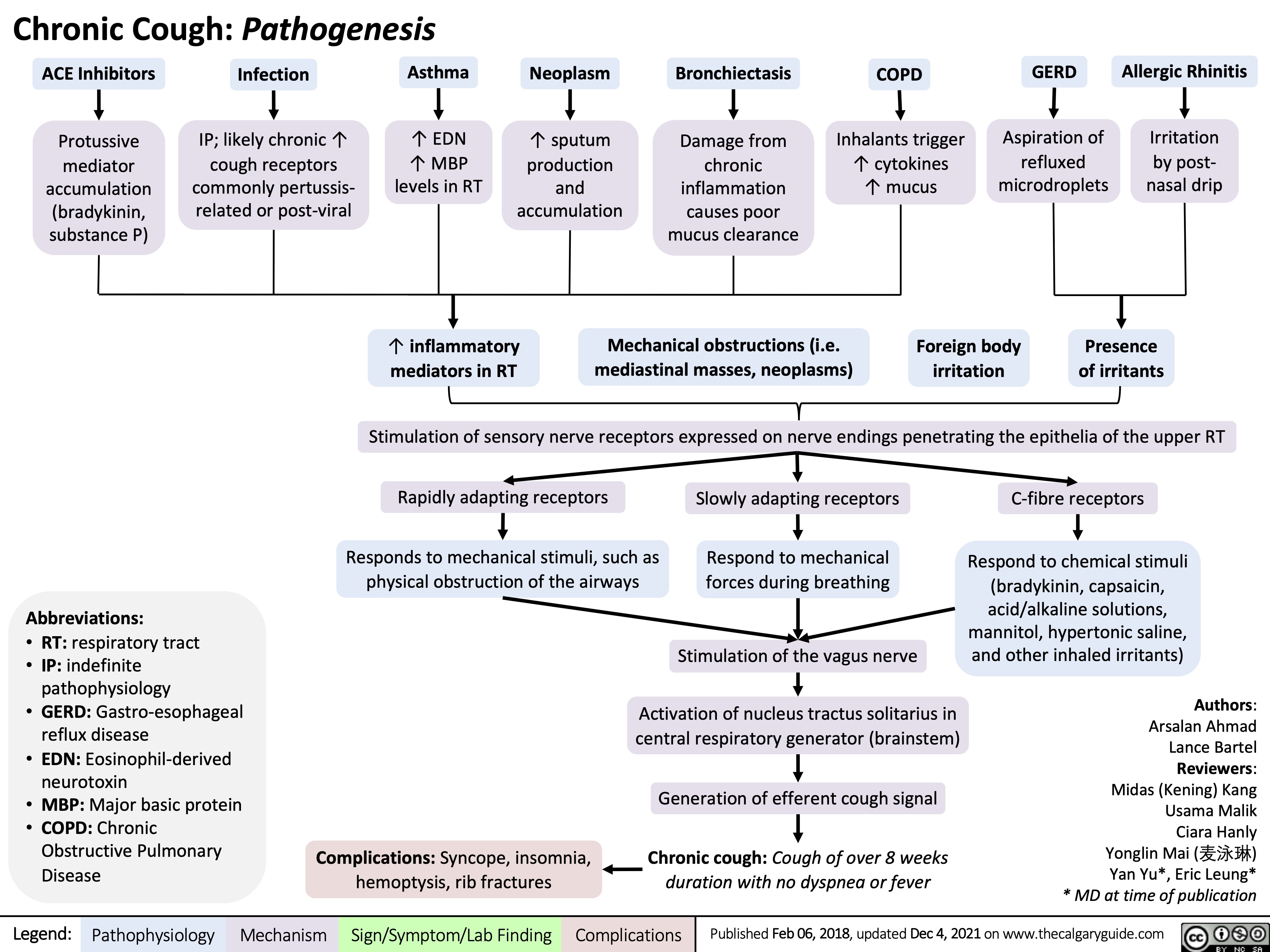
Chronic Cough Pathogenesis_2021
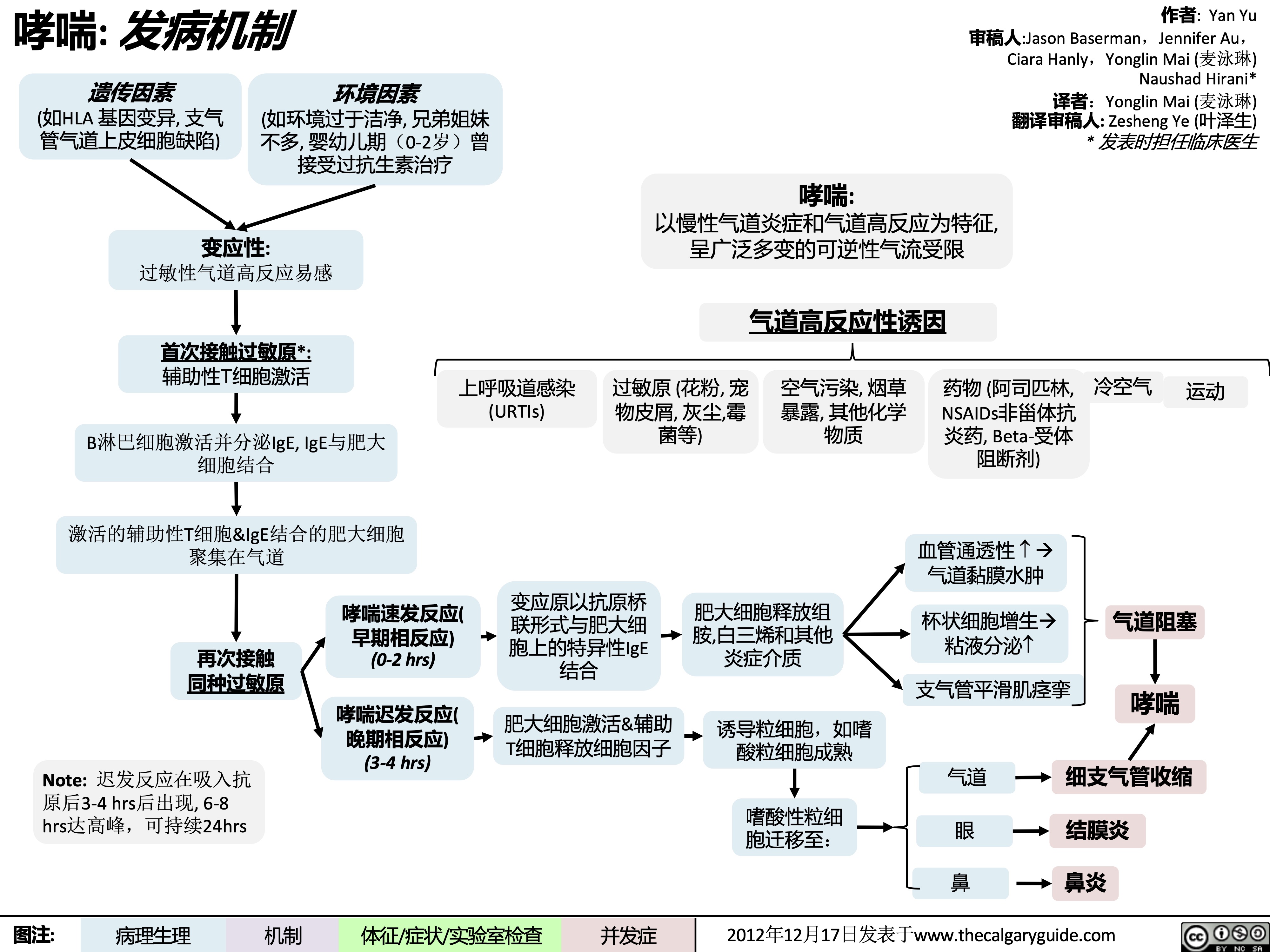
哮喘-发病机制
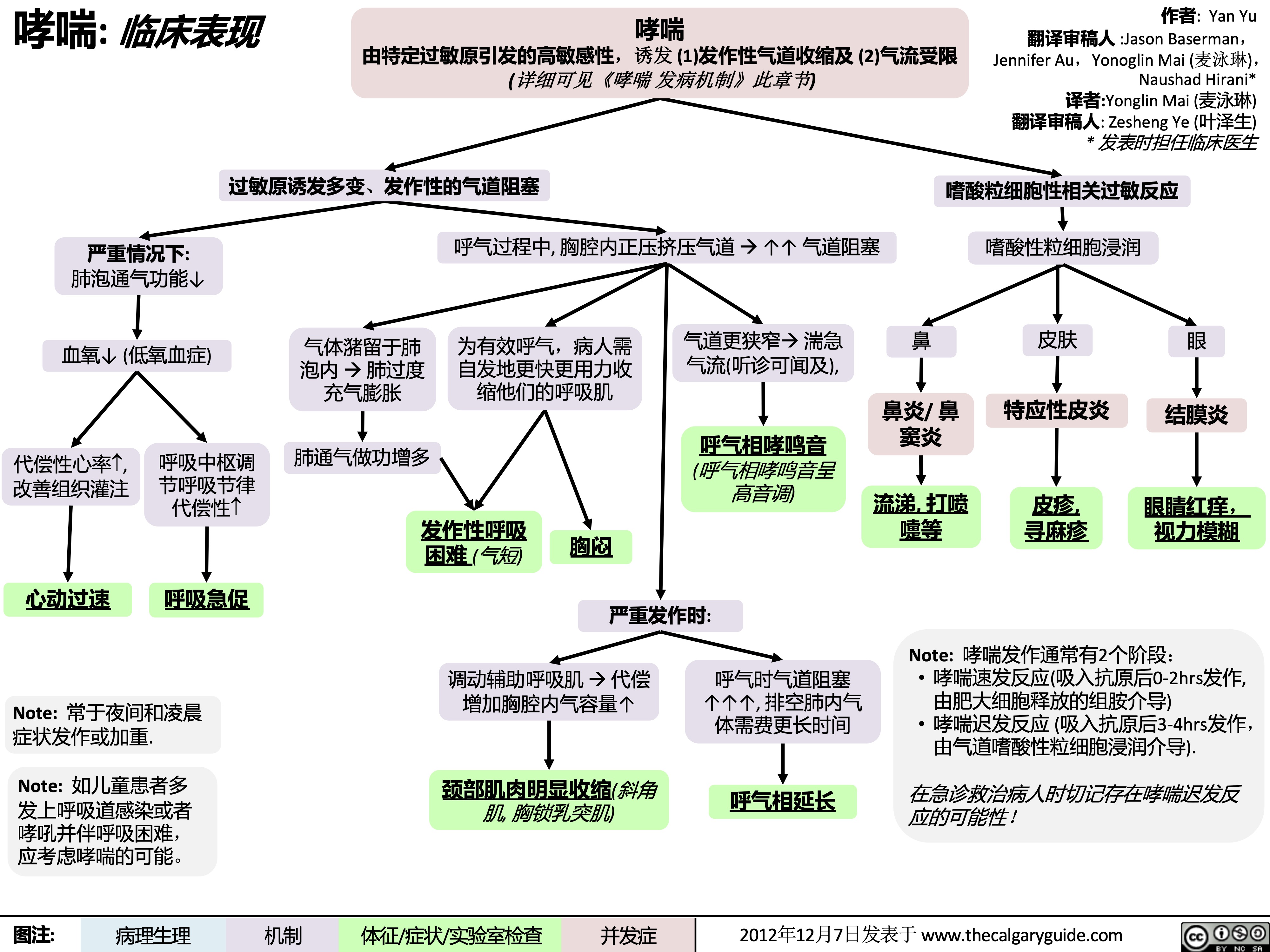
哮喘-临床表现
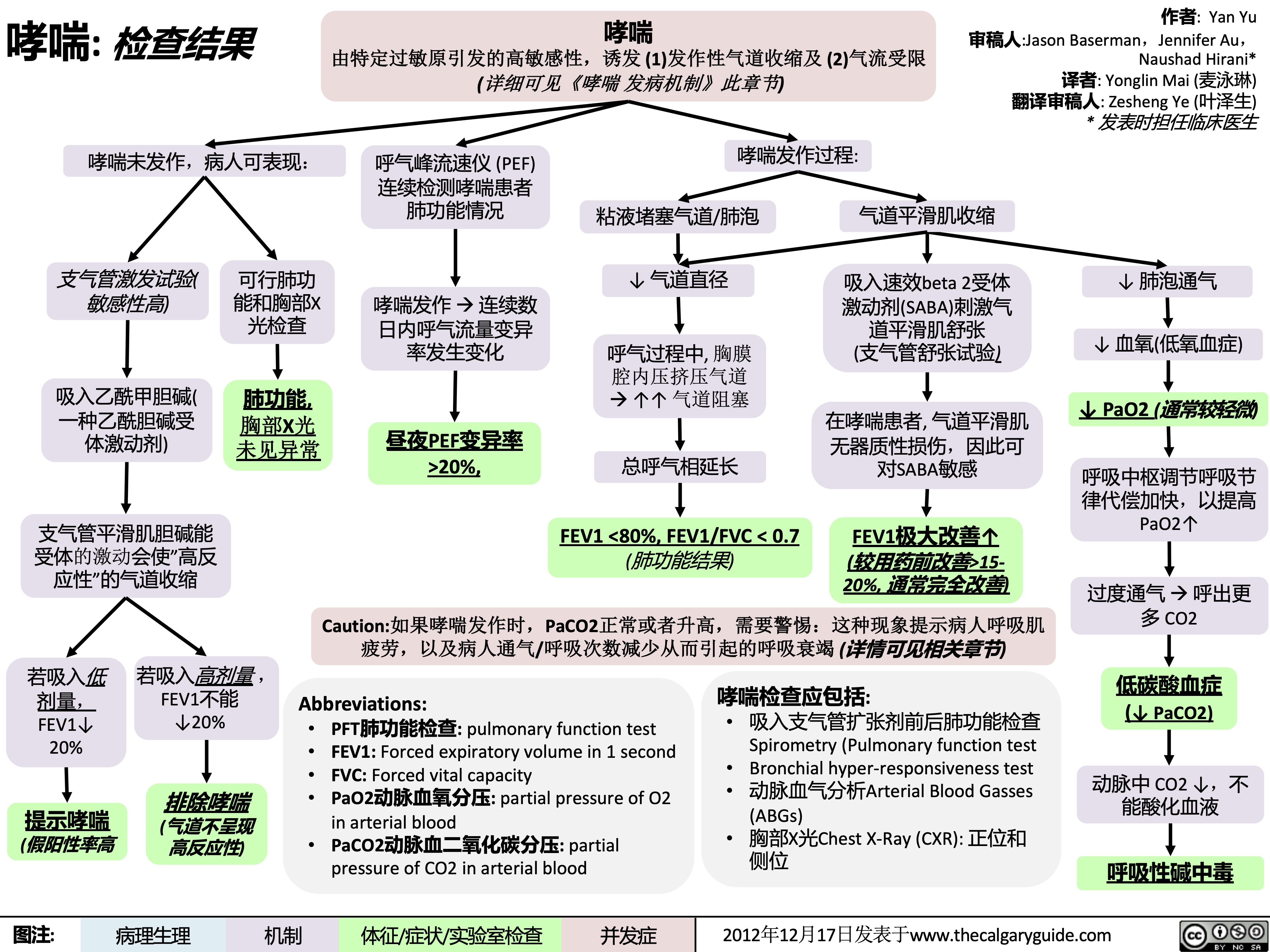
哮喘-检查结果
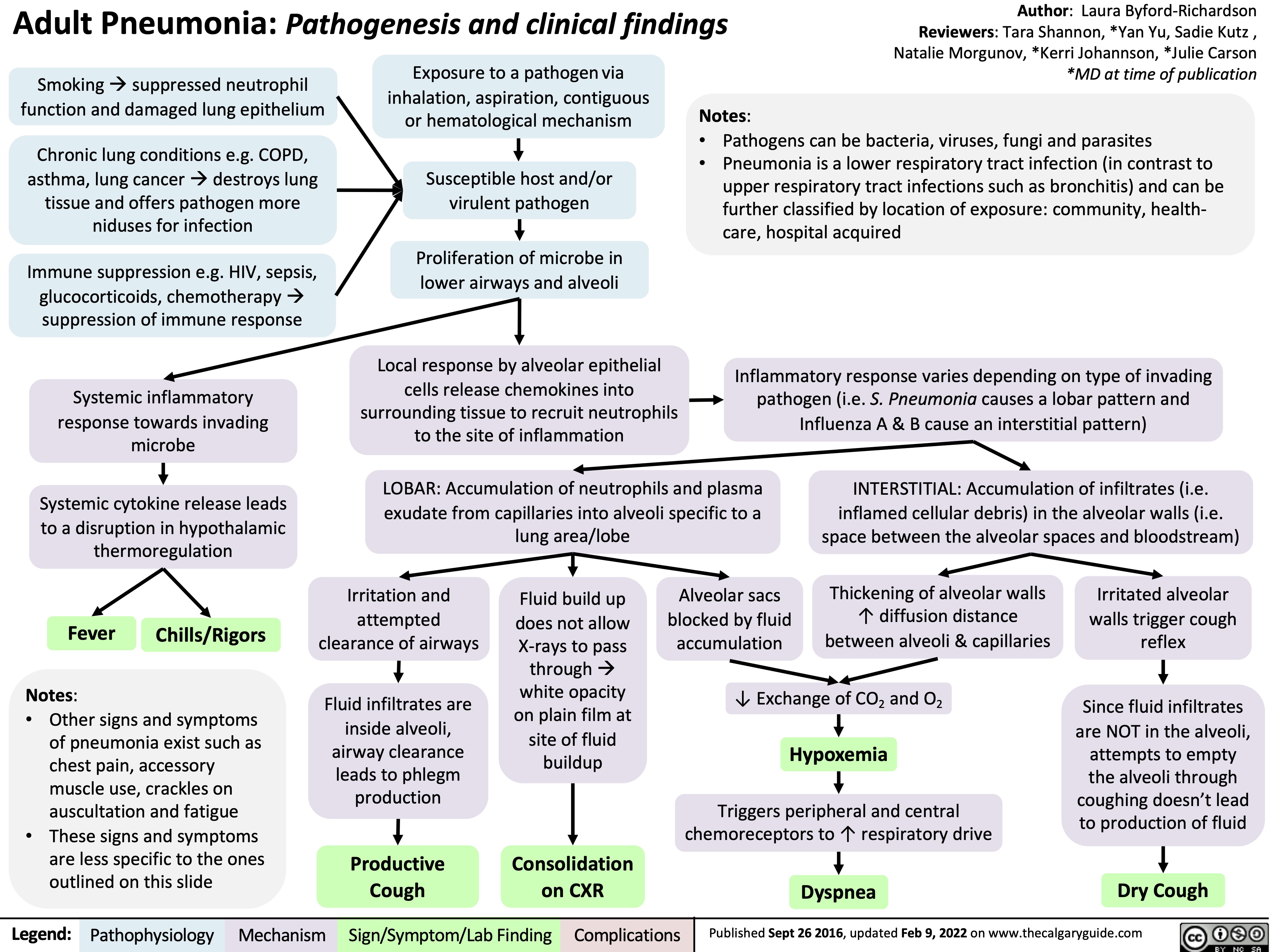
adult-pneumonia-pathogenesis-and-clinical-findings
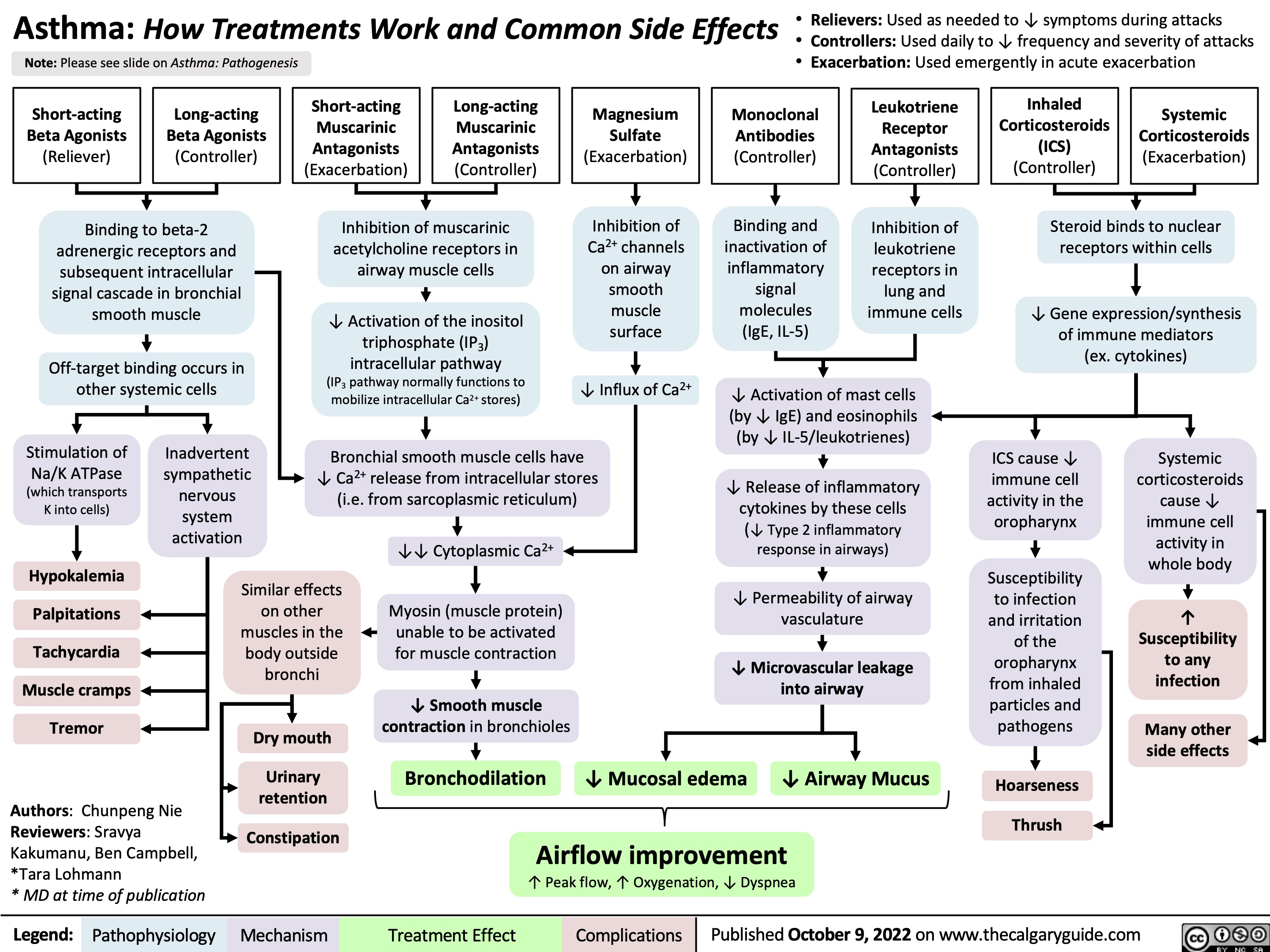
asthma-how-treatments-work-and-common-side-effects
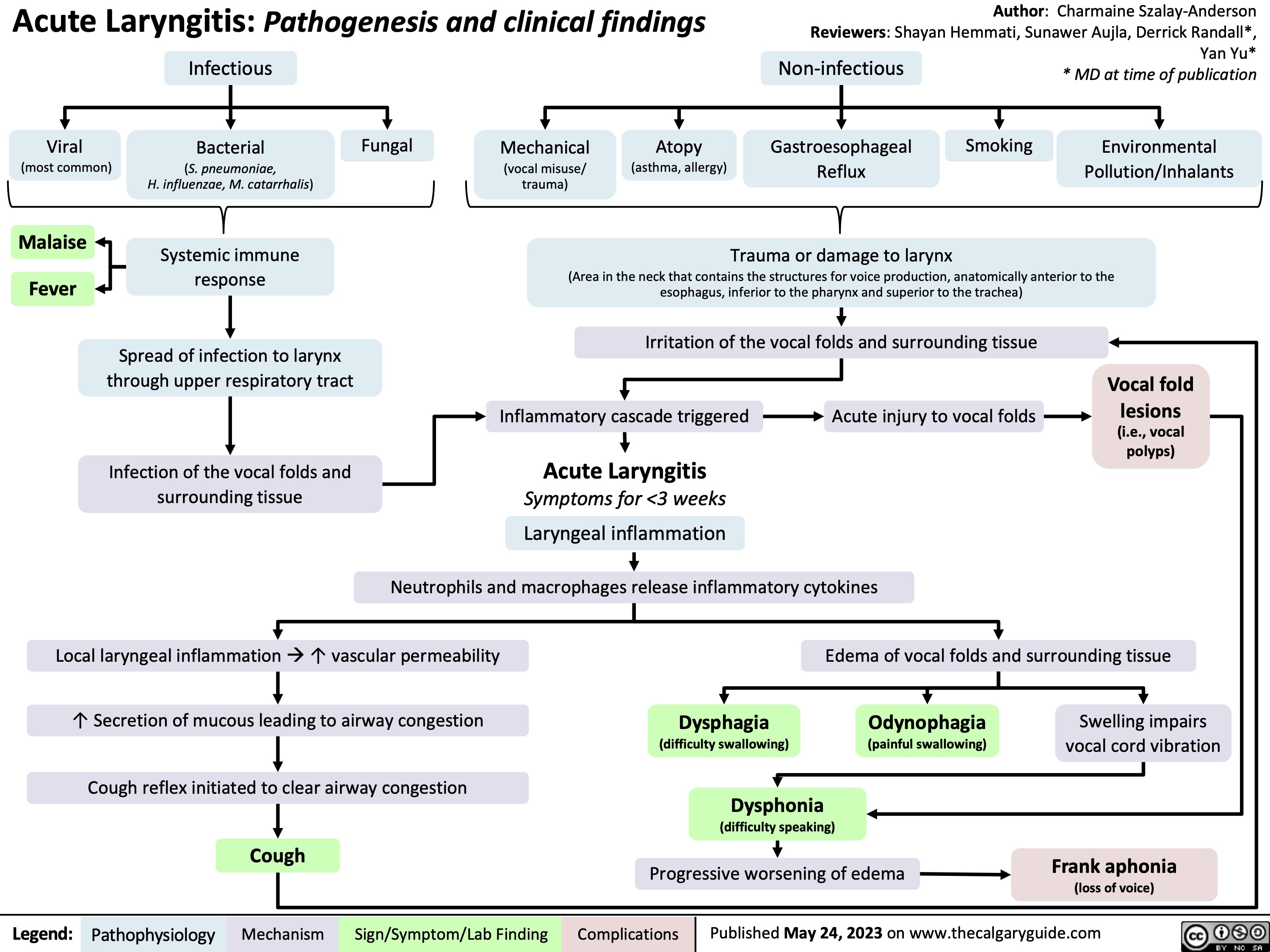
Acute Laryngitis
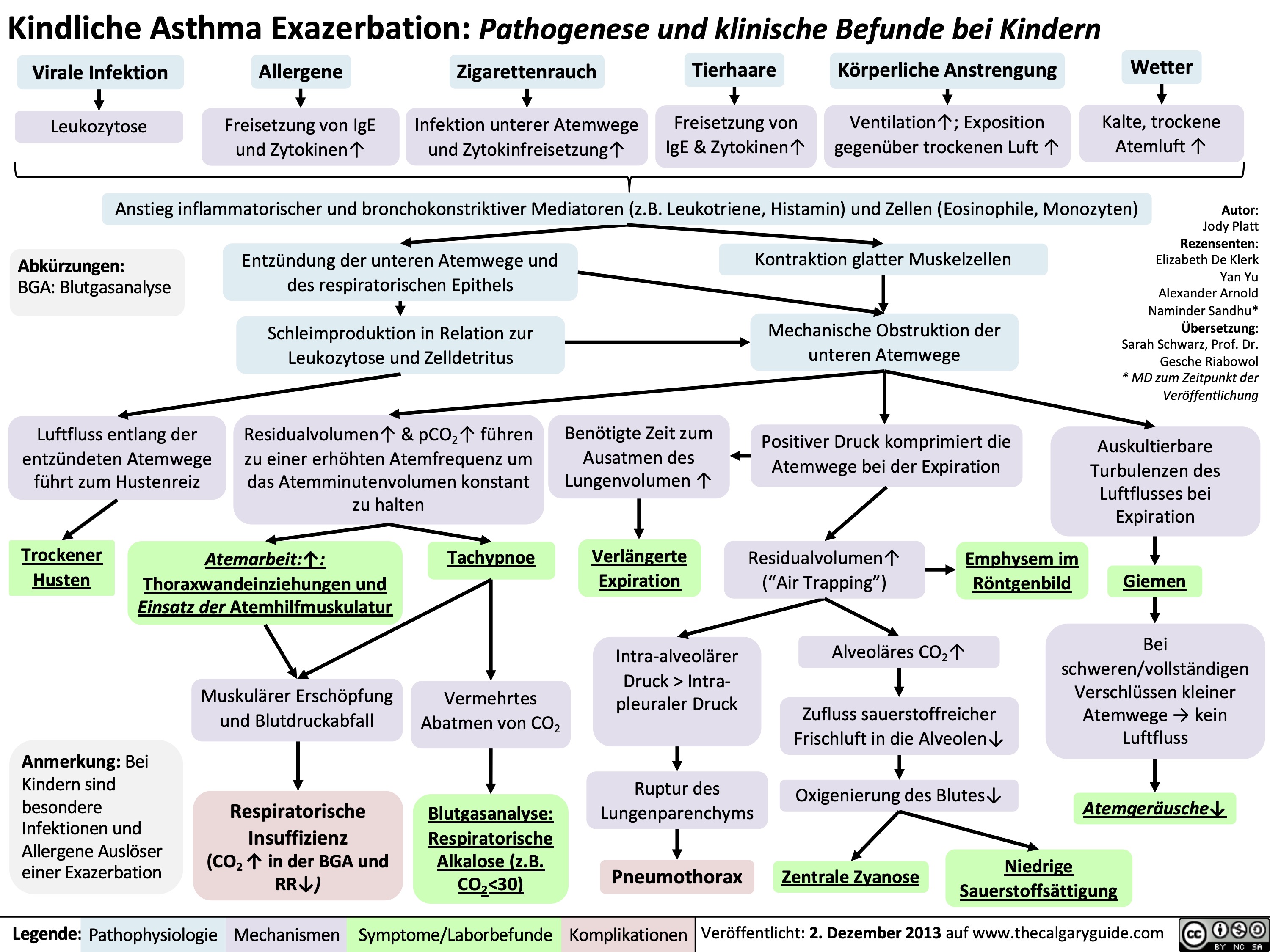
Kindliche Asthma Exazerbation: Pathogenese und klinische Befunde bei Kindern
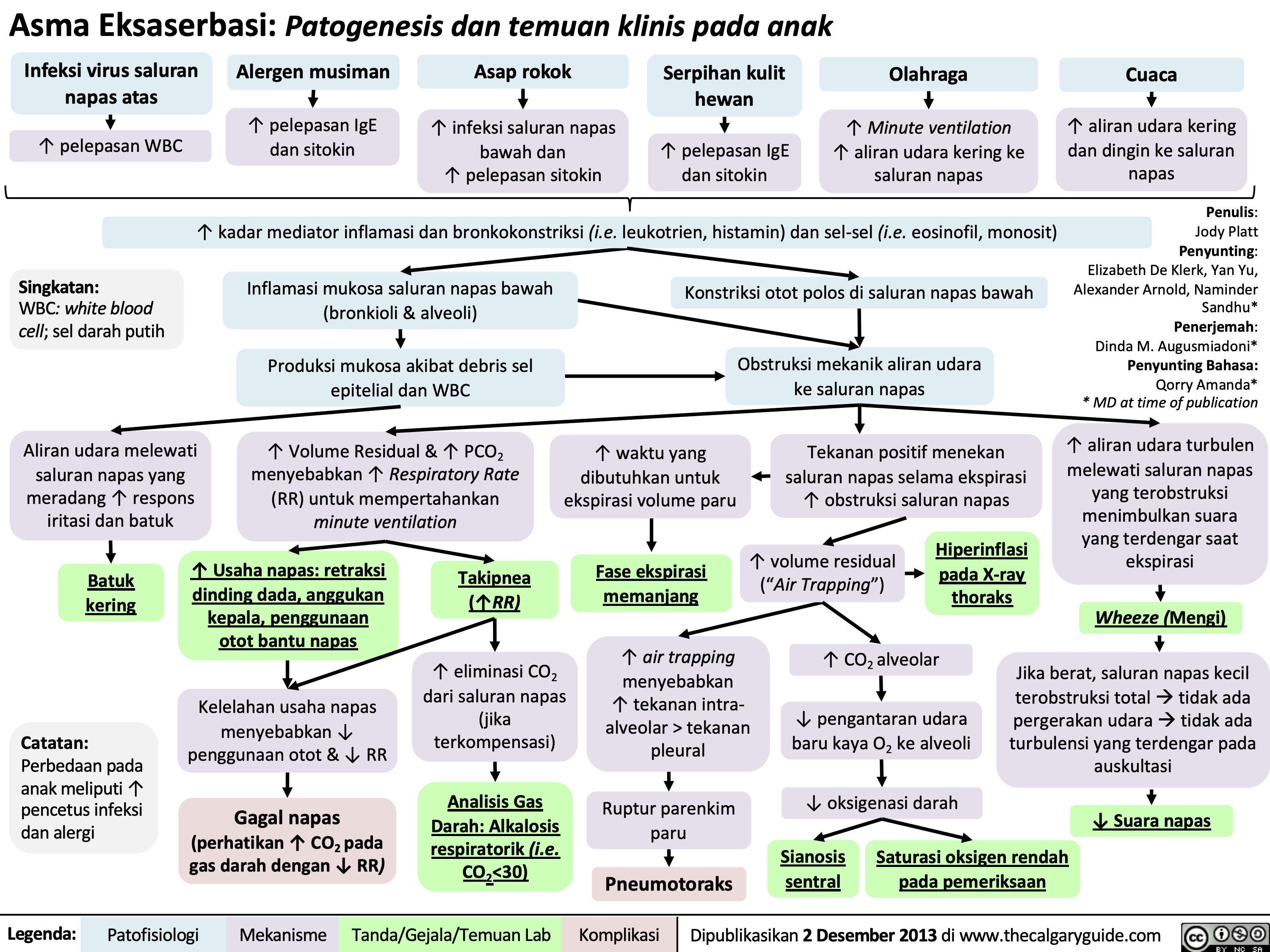
Asma Eksaserbasi Patogenesis dan temuan klinis pada anak
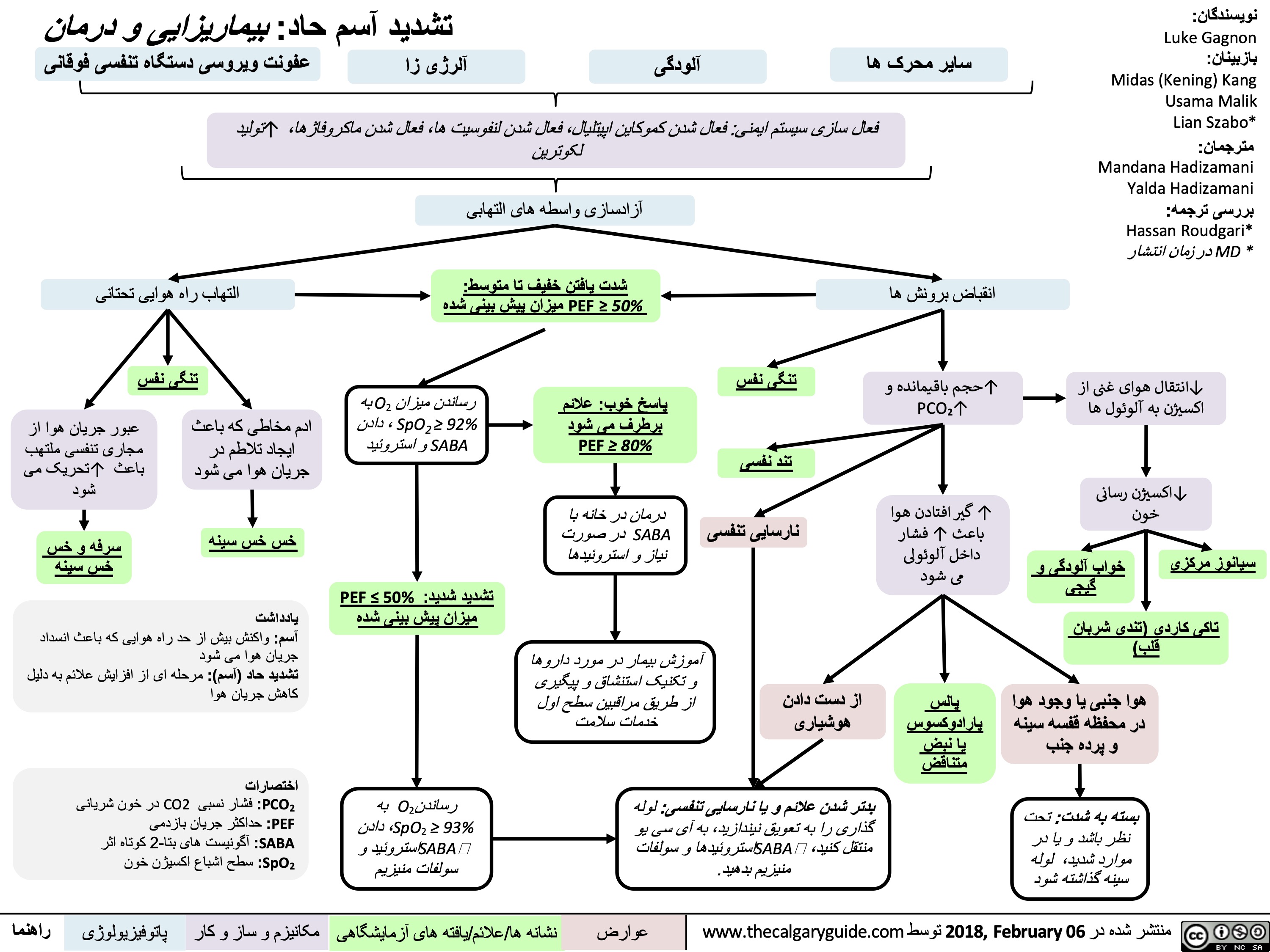
تشدید آسم حاد بیماریزایی و درمان
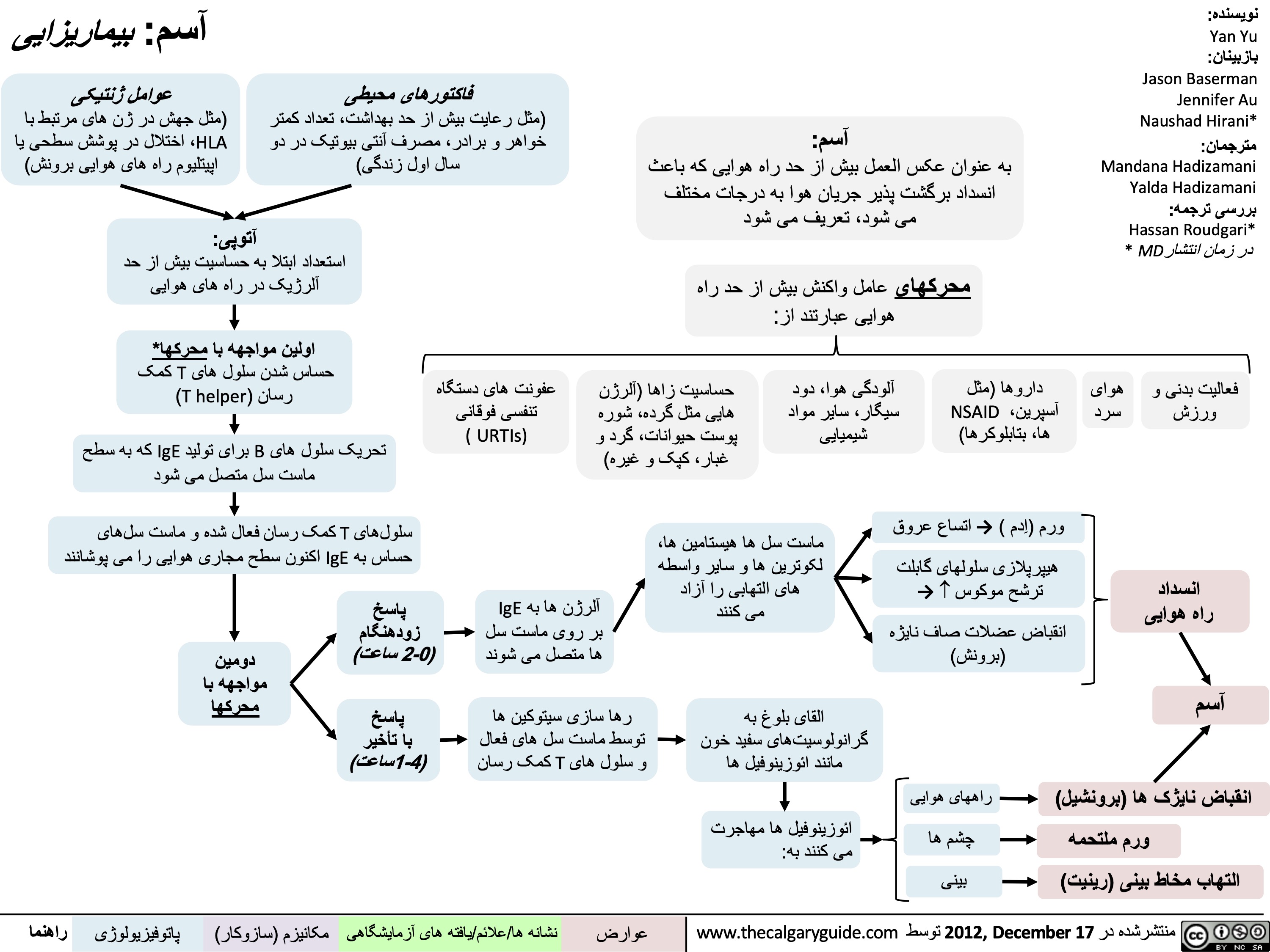
آسم بیماریزایی
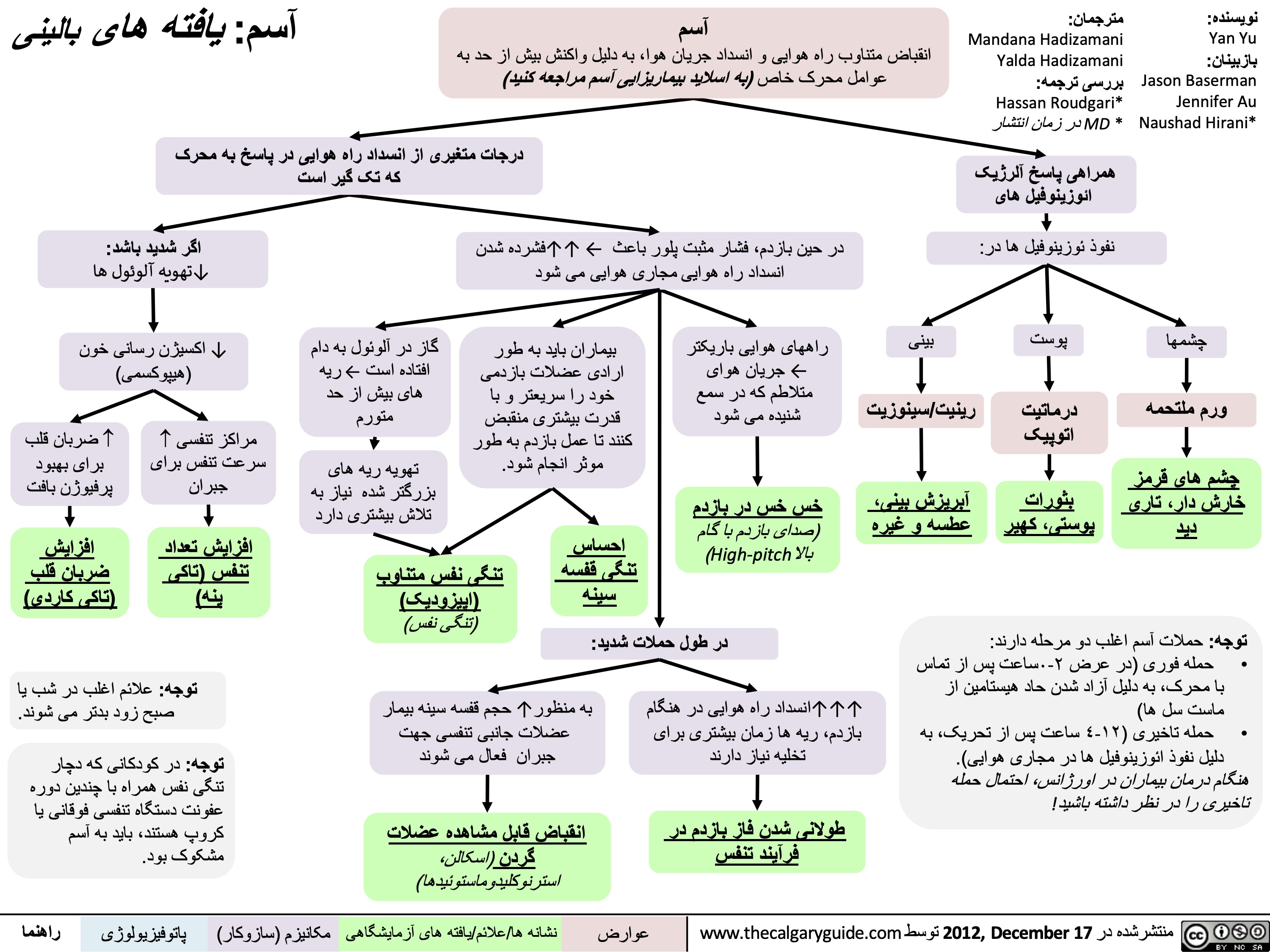
آسم یافتھ ھای بالینی
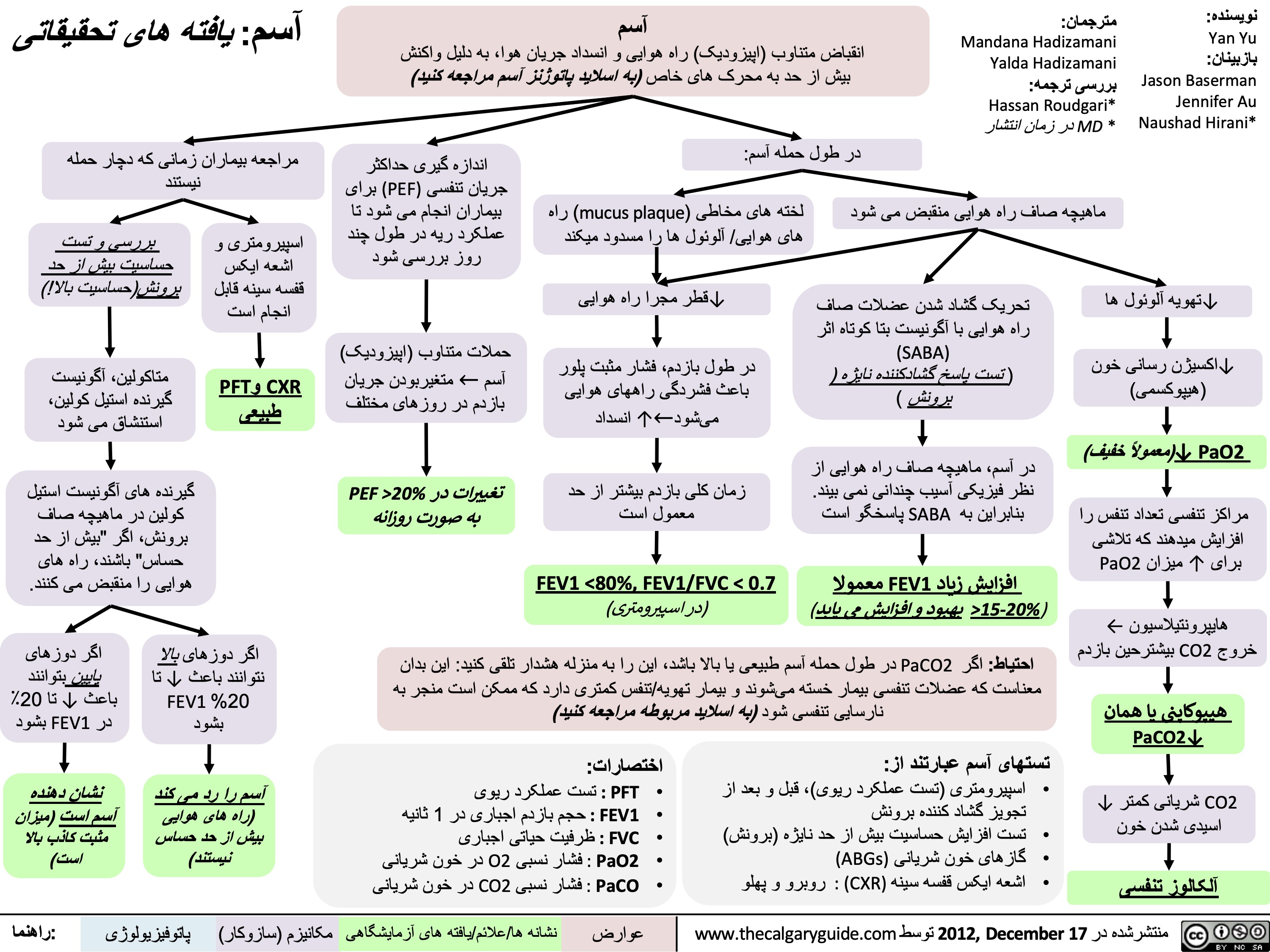
آسم یافتھ ھای تحقیقاتی
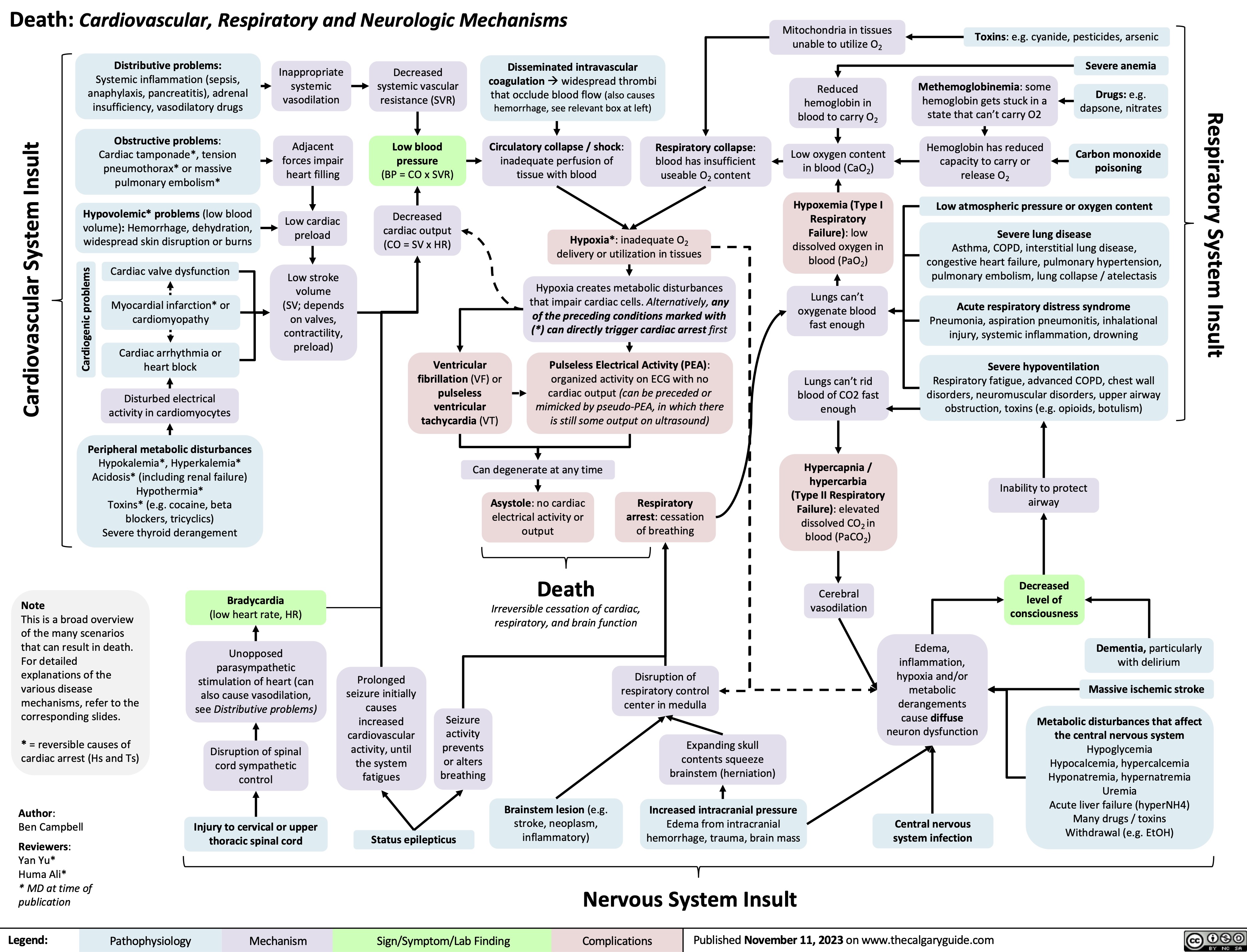
Death Cardiovascular Respiratory and Neurologic Mechanisms
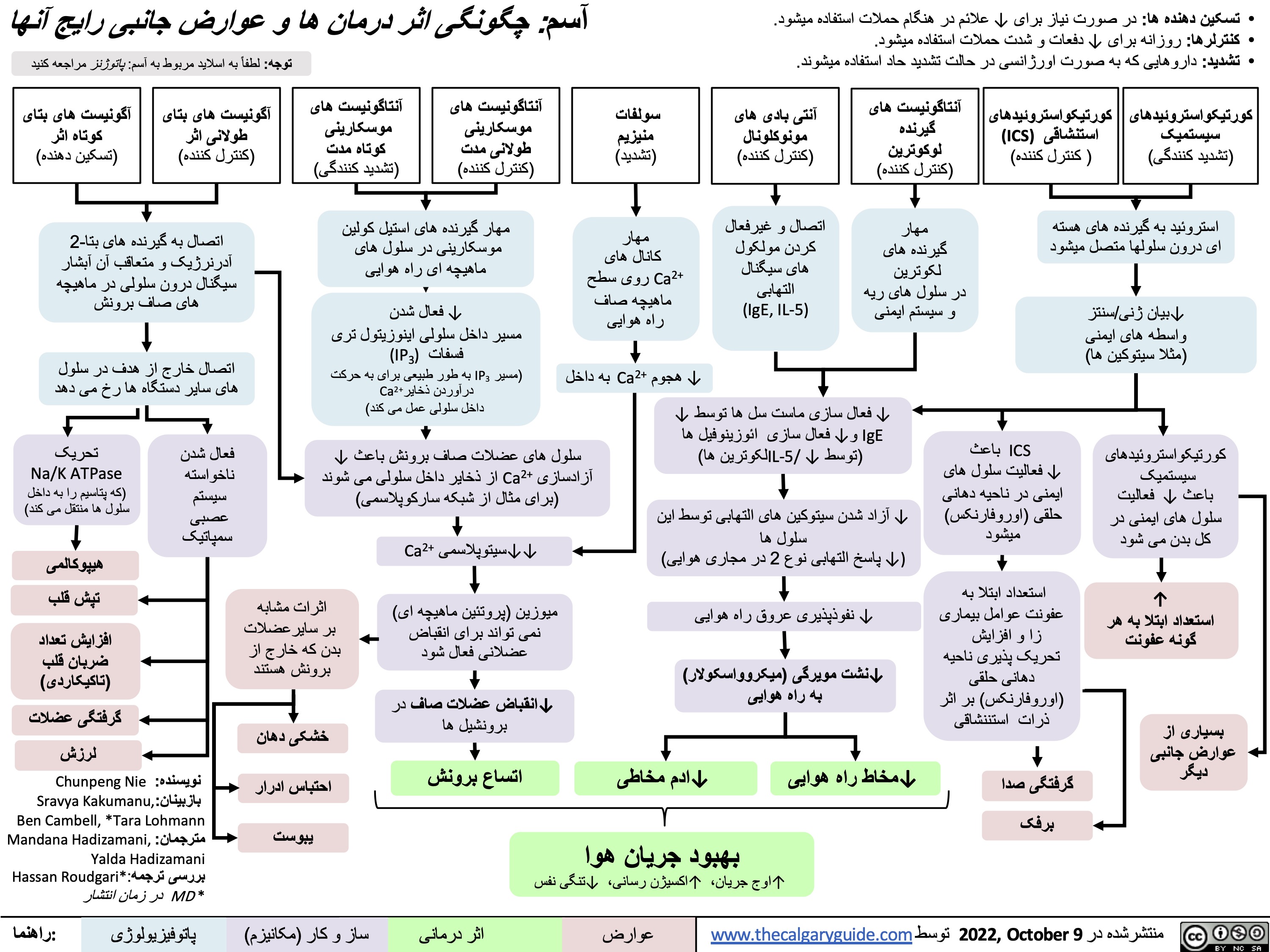
آسم-چگونگی-اثر-درمان-ھا-و-عوارض-جانبی-ر
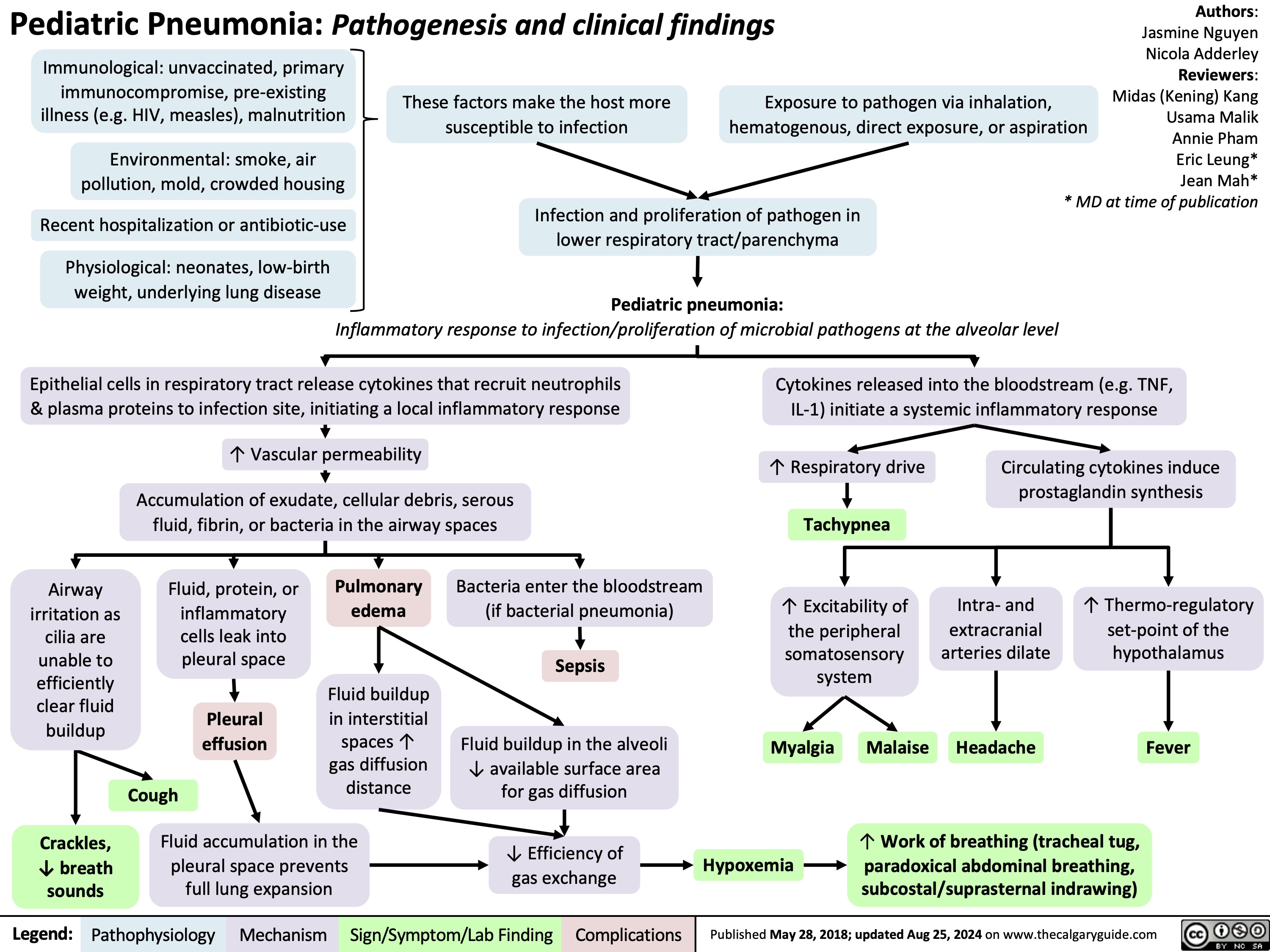
Pediatric Pneumonia Pathogenesis and Clinical Findings
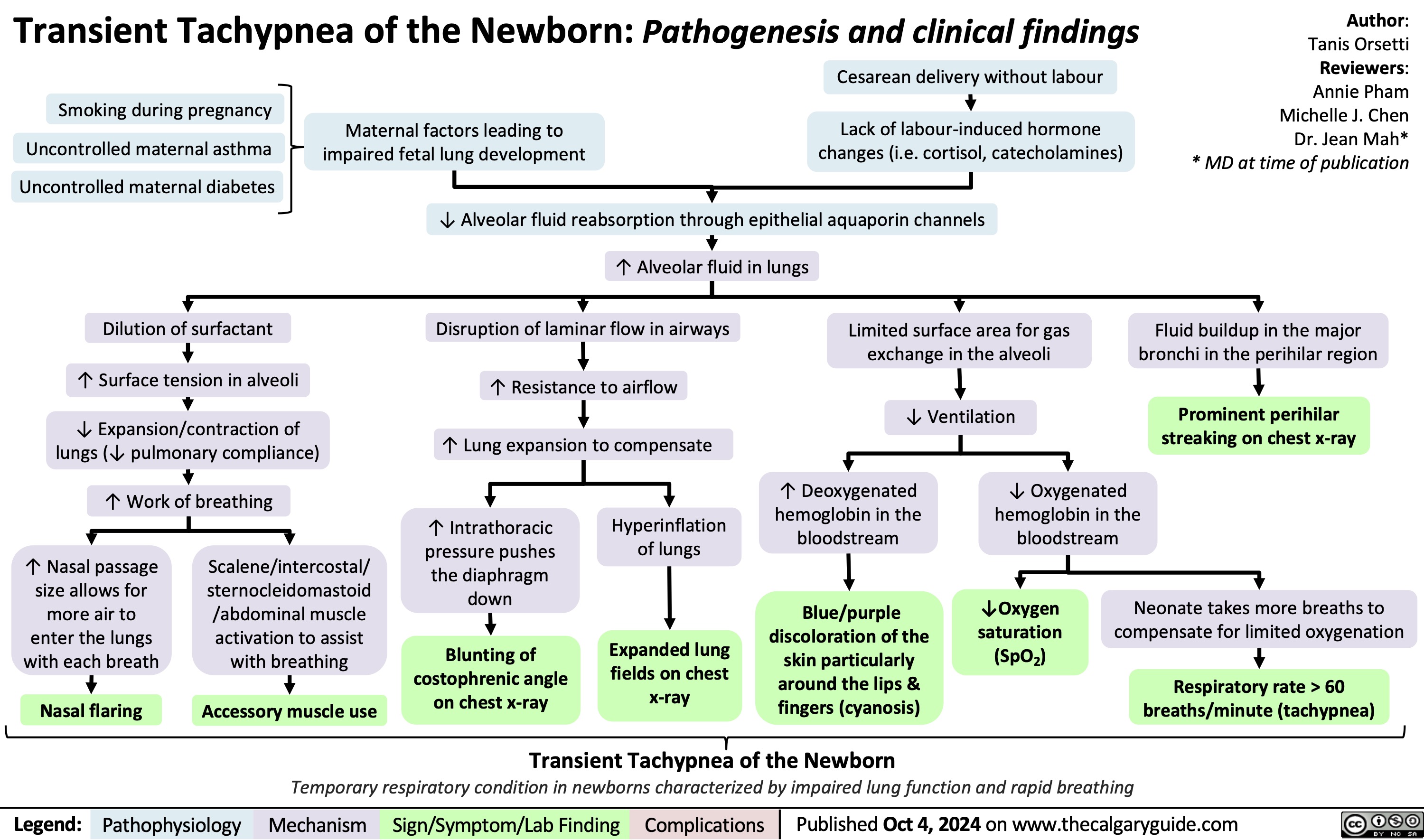
Transient Tachypnea of the Newborn
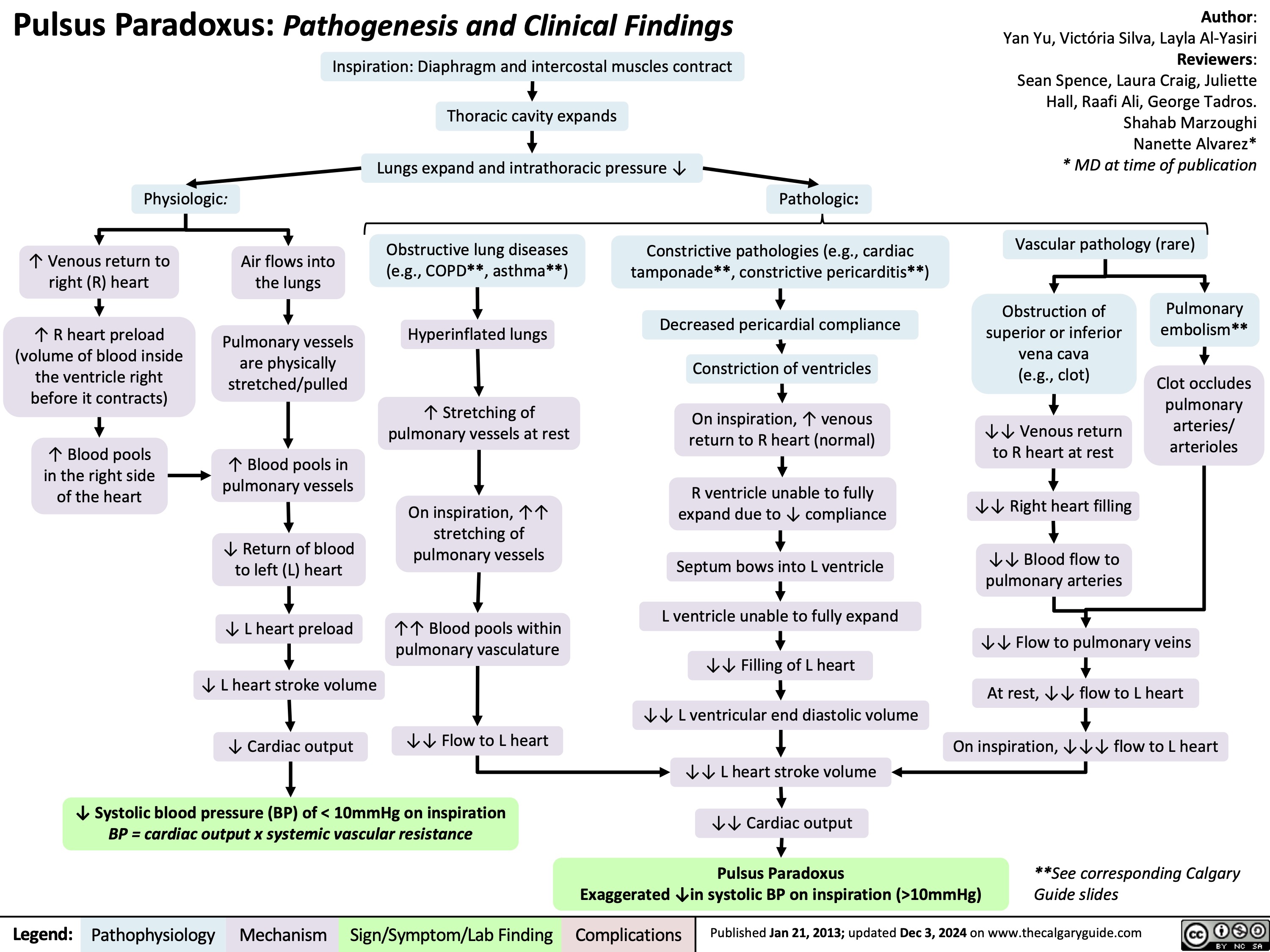
Pulsus Paradoxus
Pediatric Asthma Exacerbations

