SEARCH RESULTS FOR: tamponade
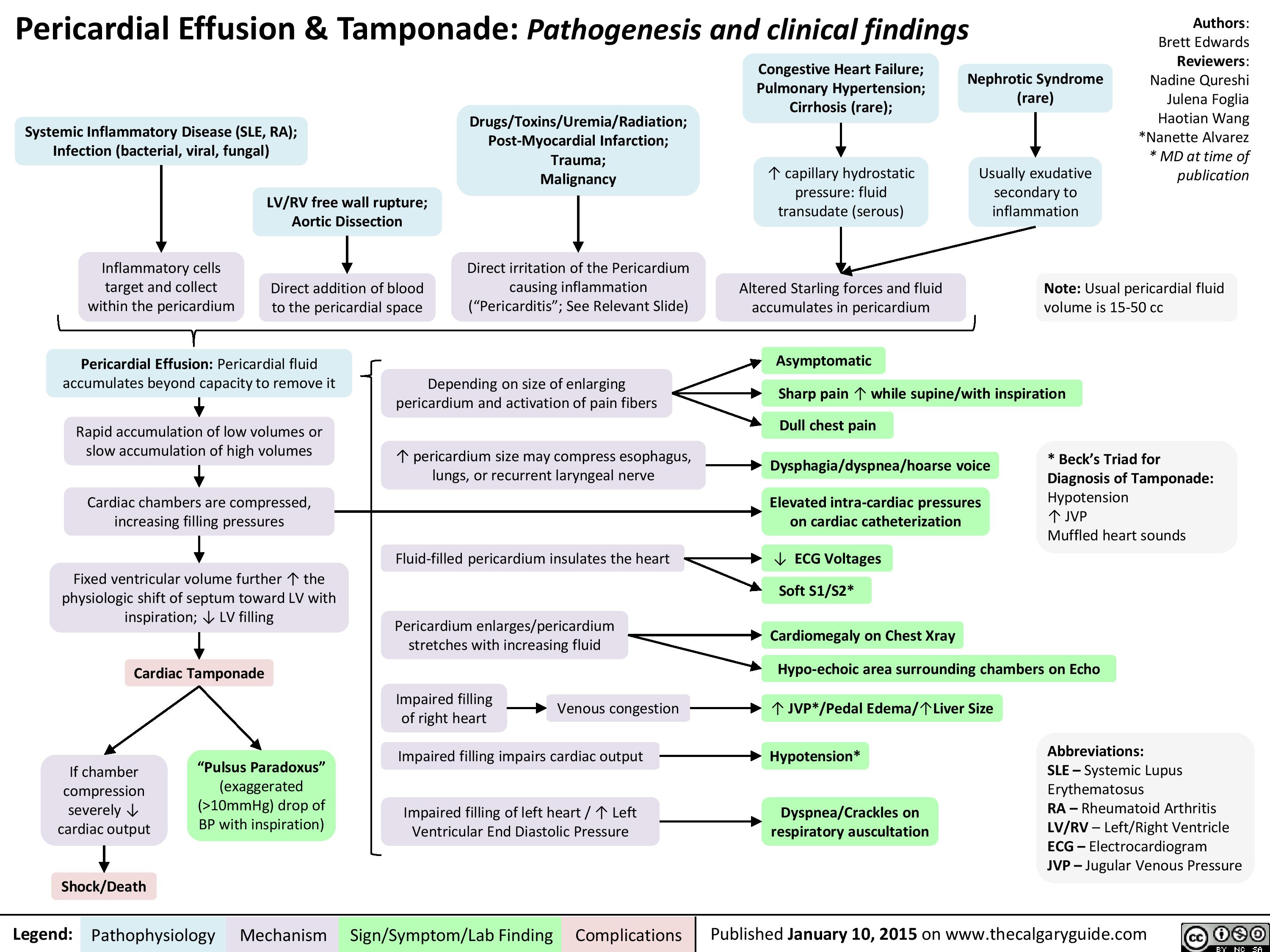
Pericardial Effusion and Tamponade: Pathogenesis and Clinical Findings
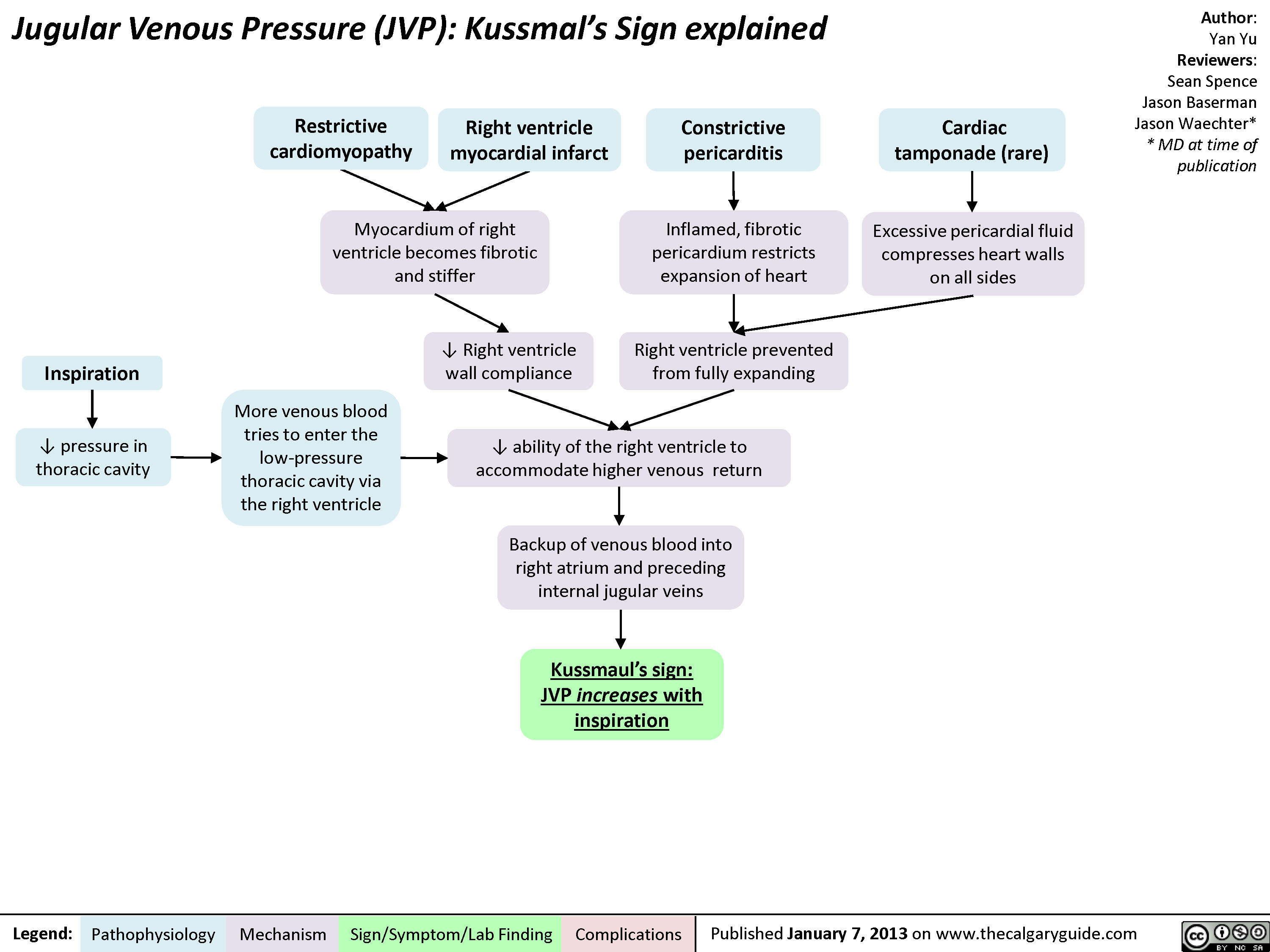
jvp-kussmals-sign-explained
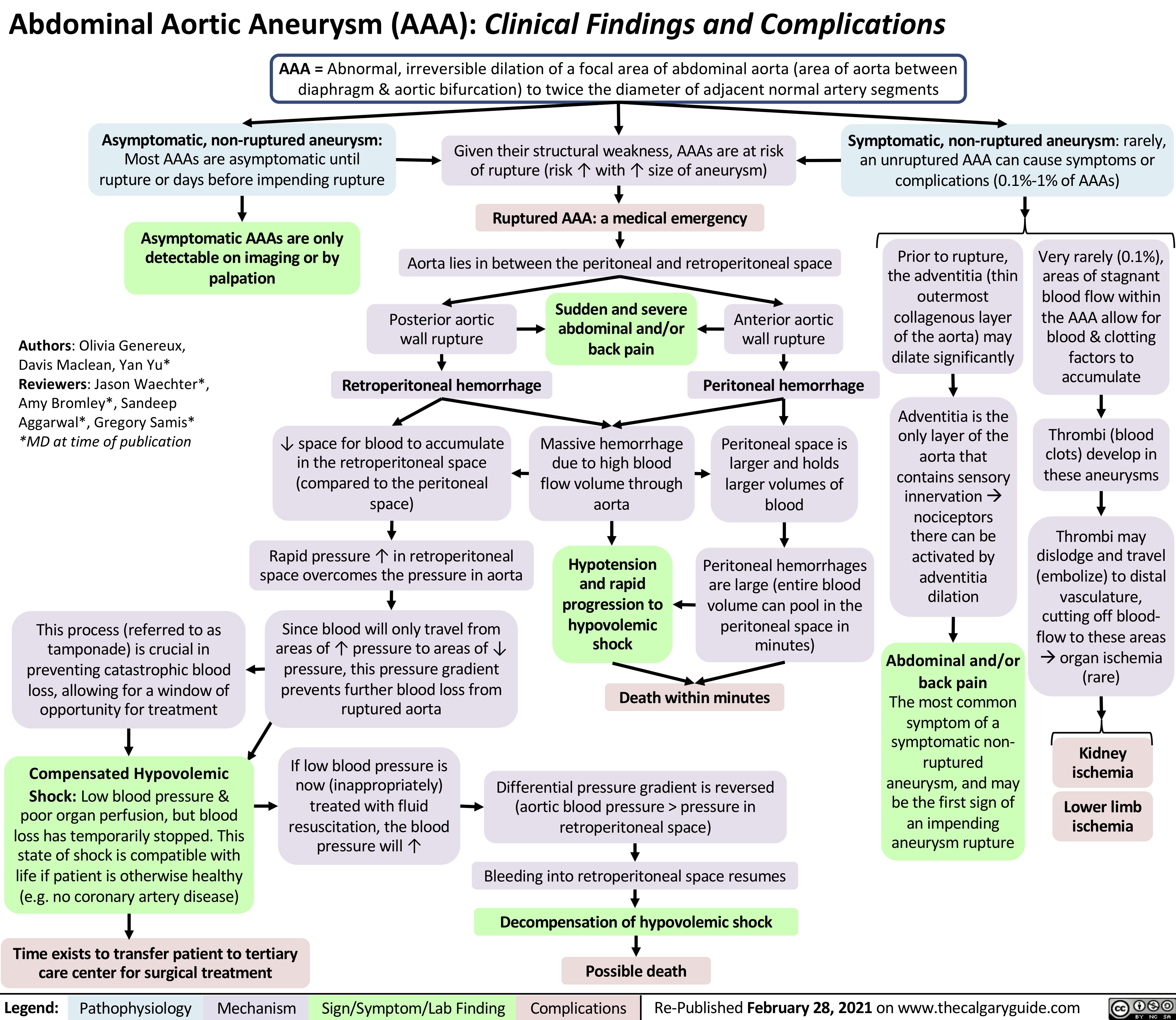
AAA-Clinical-Findings-and-Complications
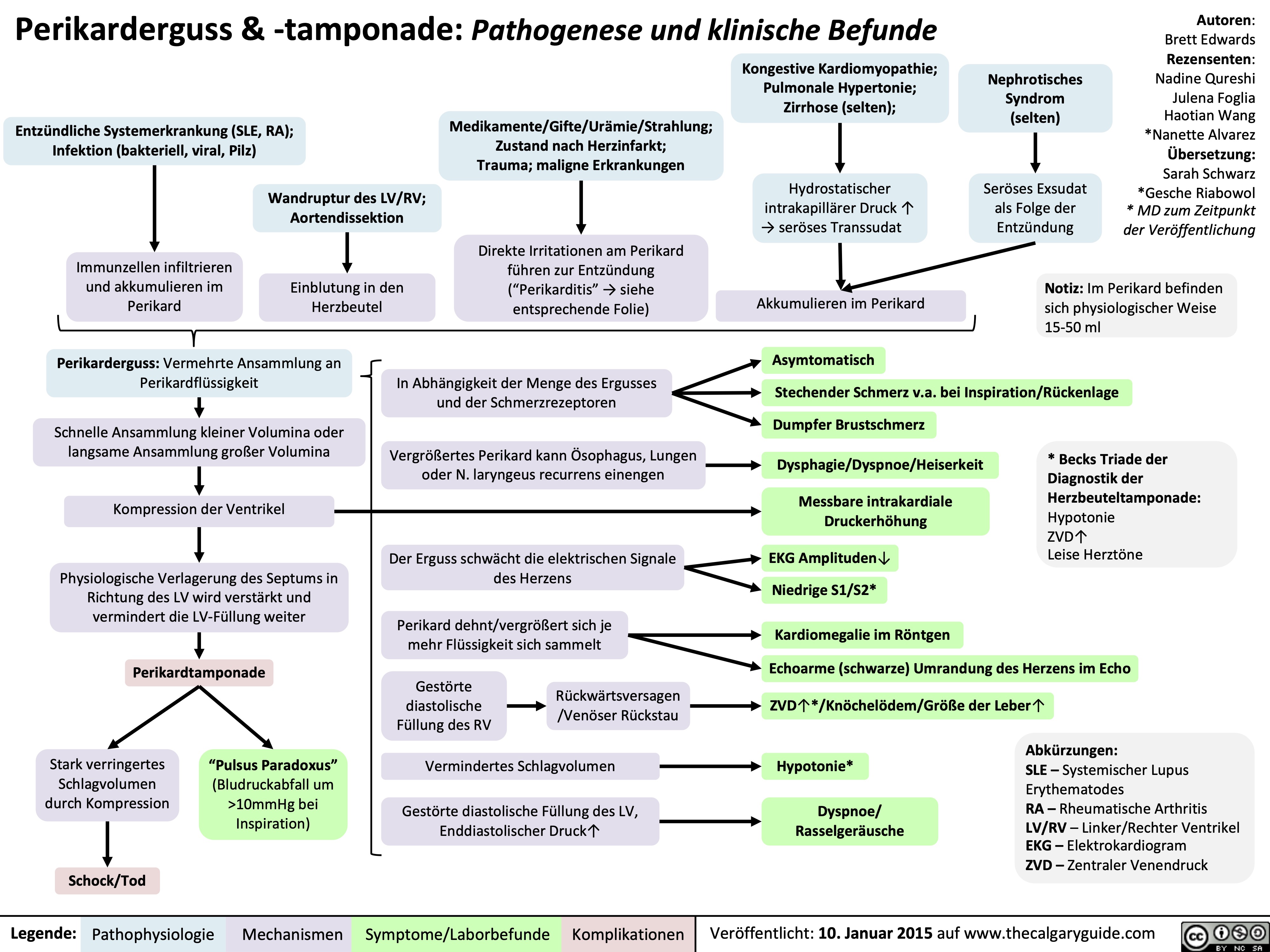
perikarderguss-tamponade-pathogenese-und-klinische-befunde
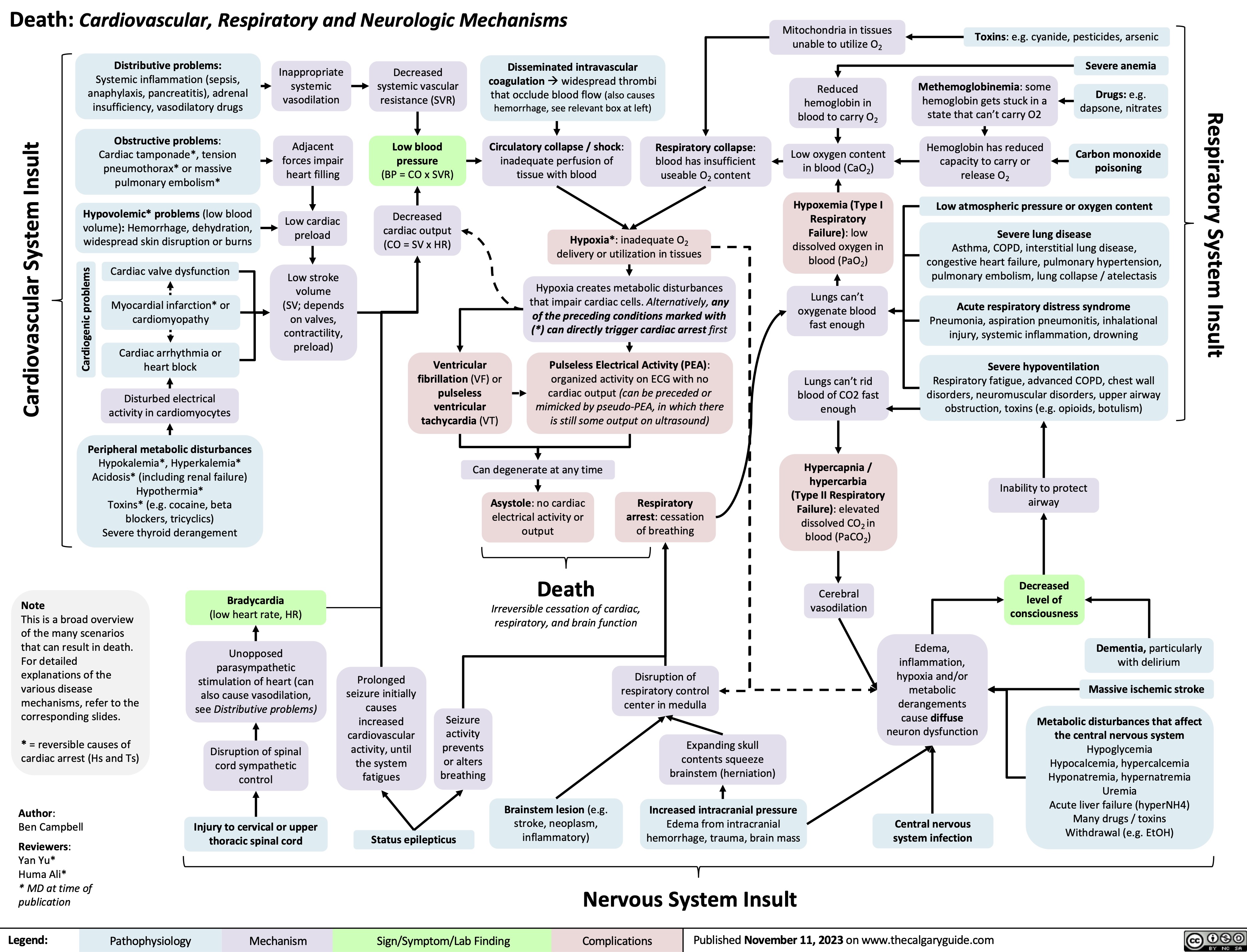
Death Cardiovascular Respiratory and Neurologic Mechanisms
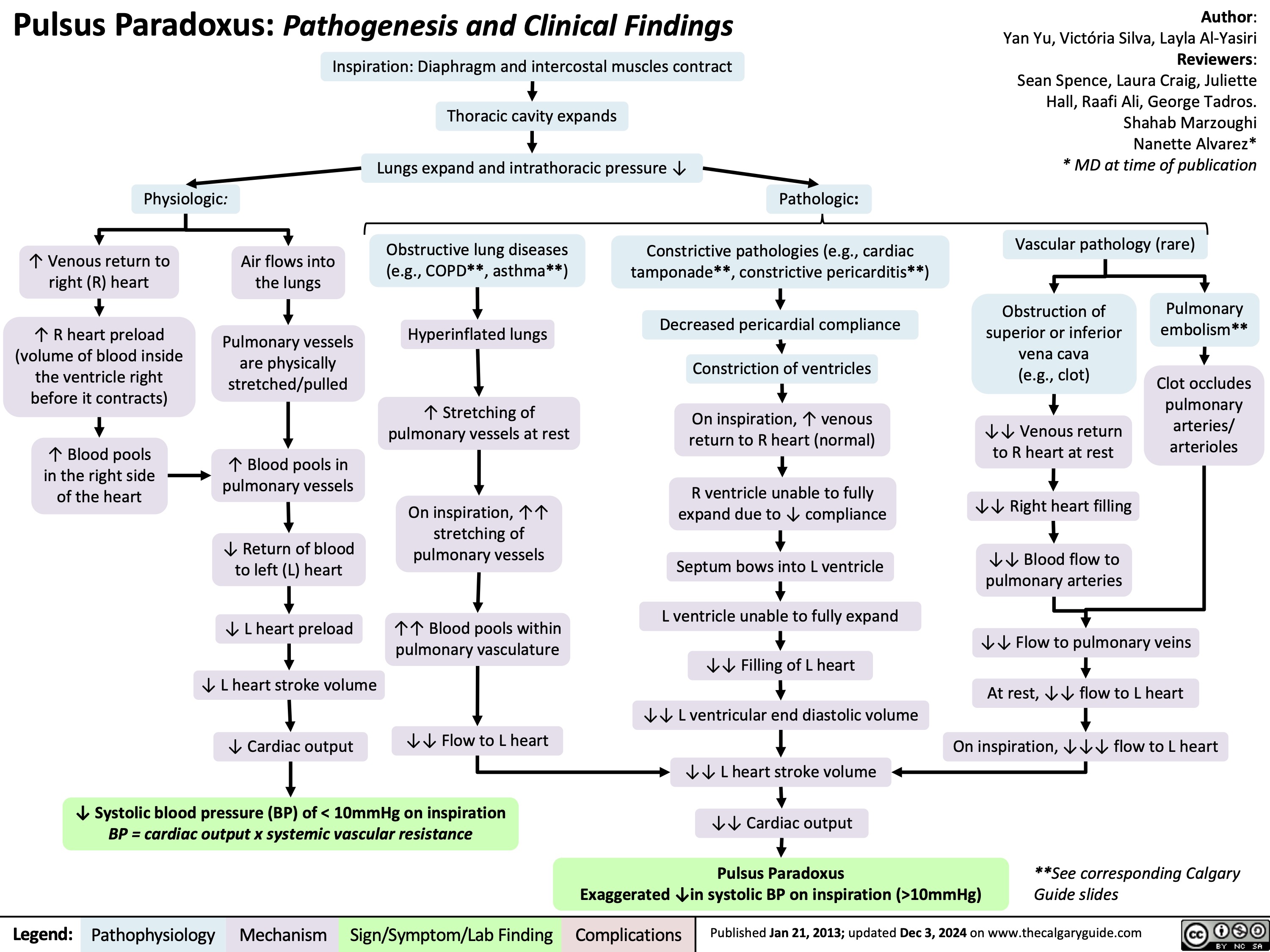
Pulsus Paradoxus
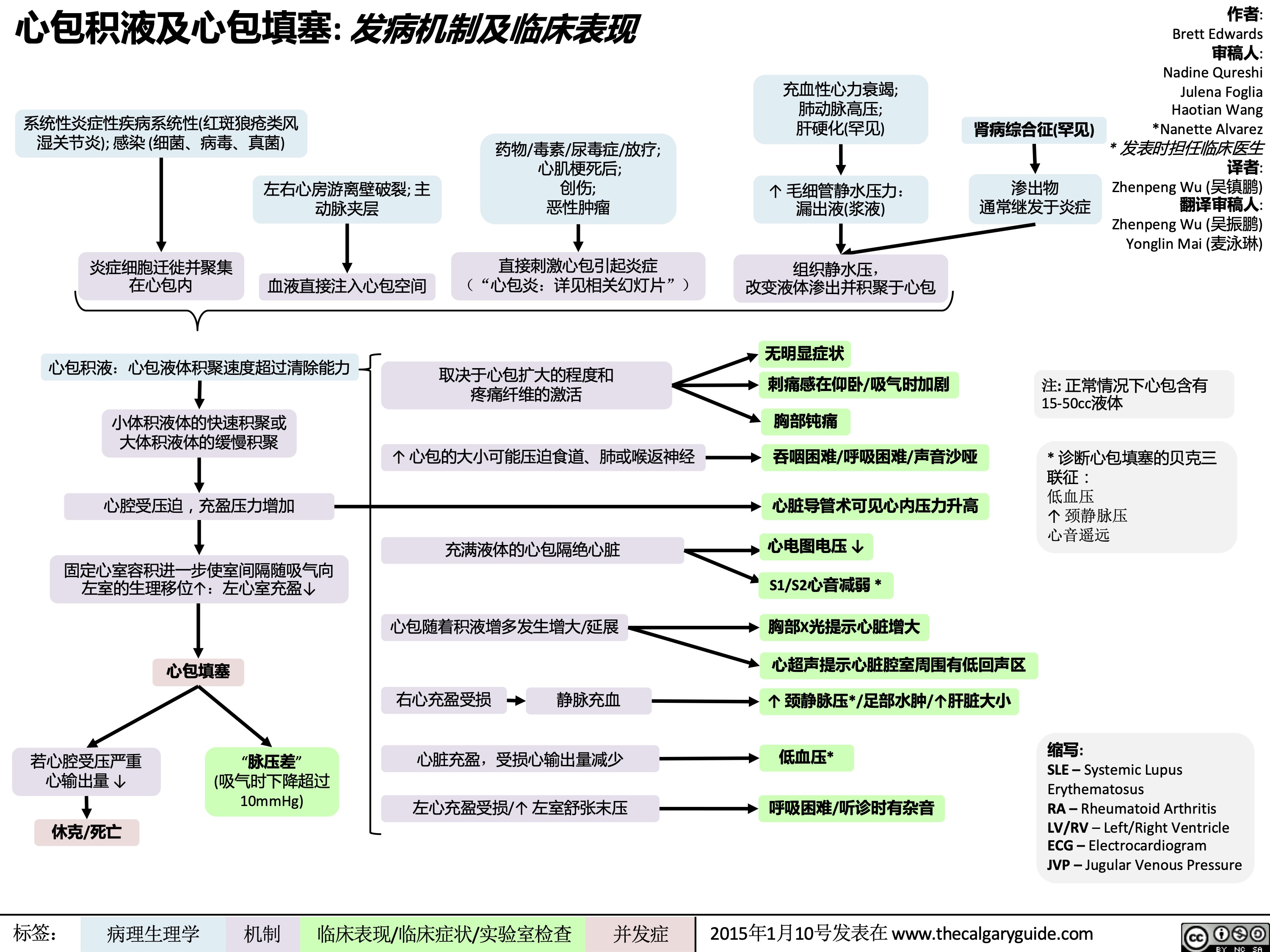
心包积液及心包填塞
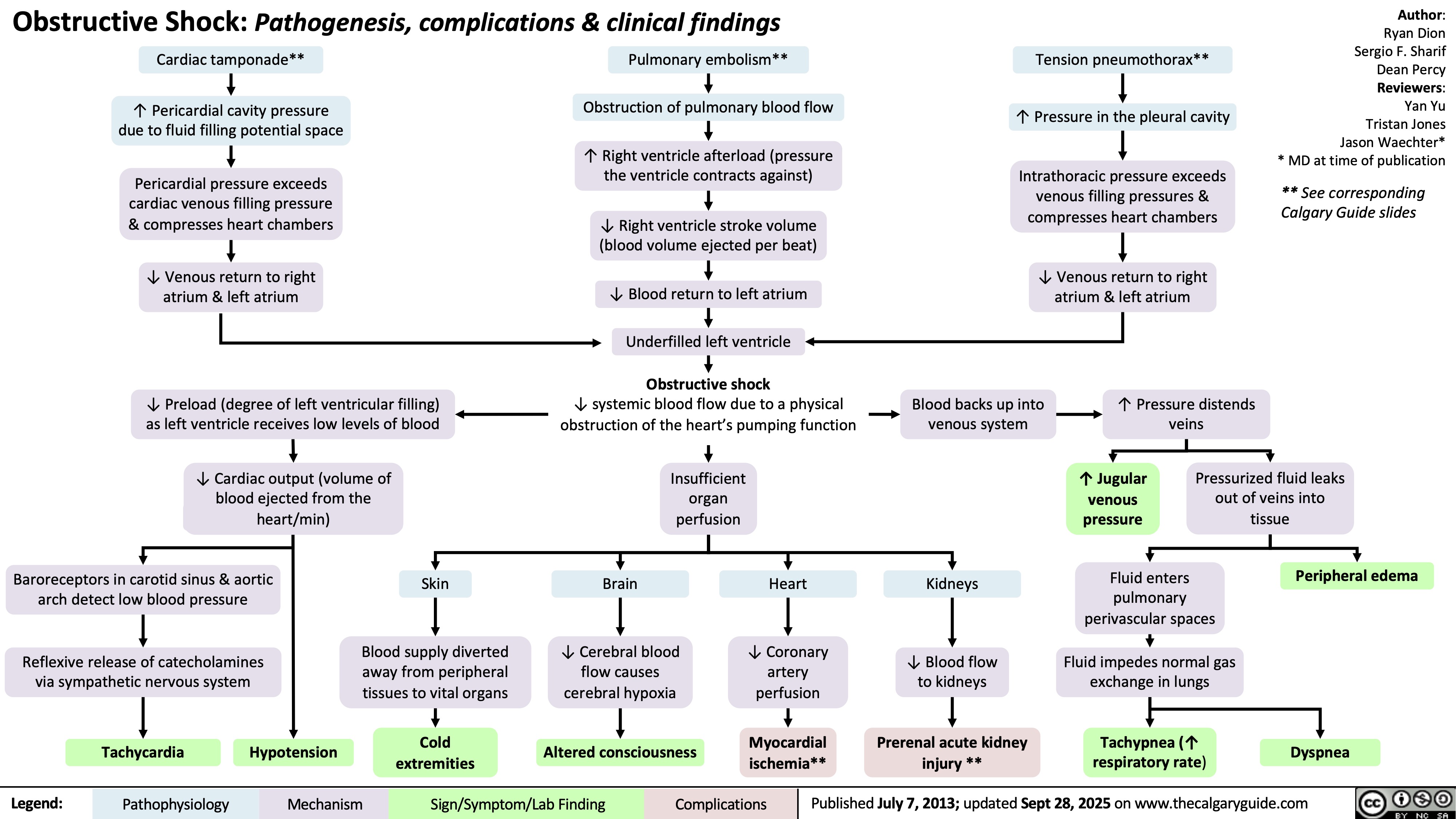
Obstructive Shock