SEARCH RESULTS FOR: Acute-Respiratory-Distress-Syndrome
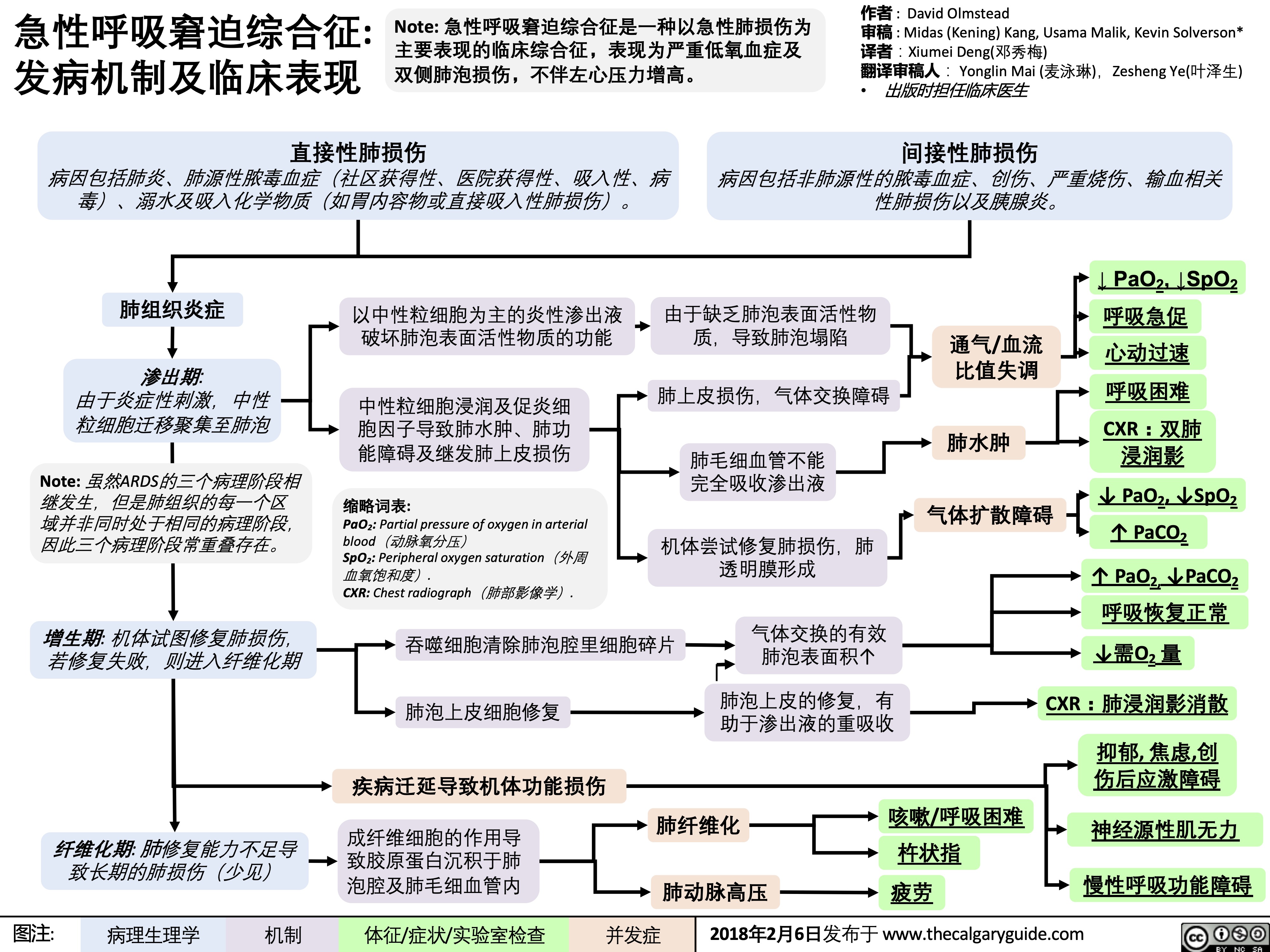
急性呼吸窘迫综合征: 发病机制及临床表现
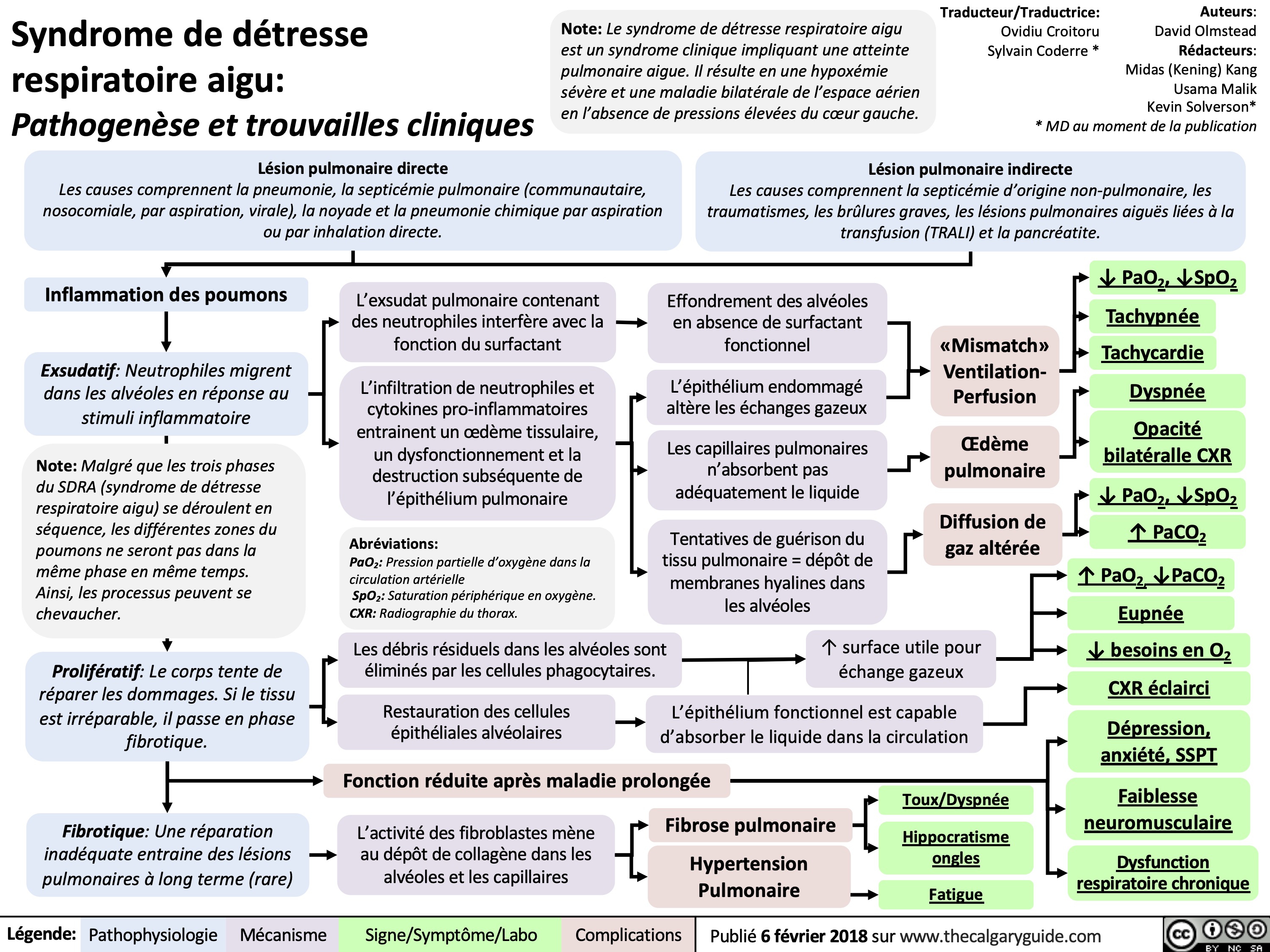
Syndrome de détresse respiratoire aigu: Pathogenèse et trouvailles cliniques
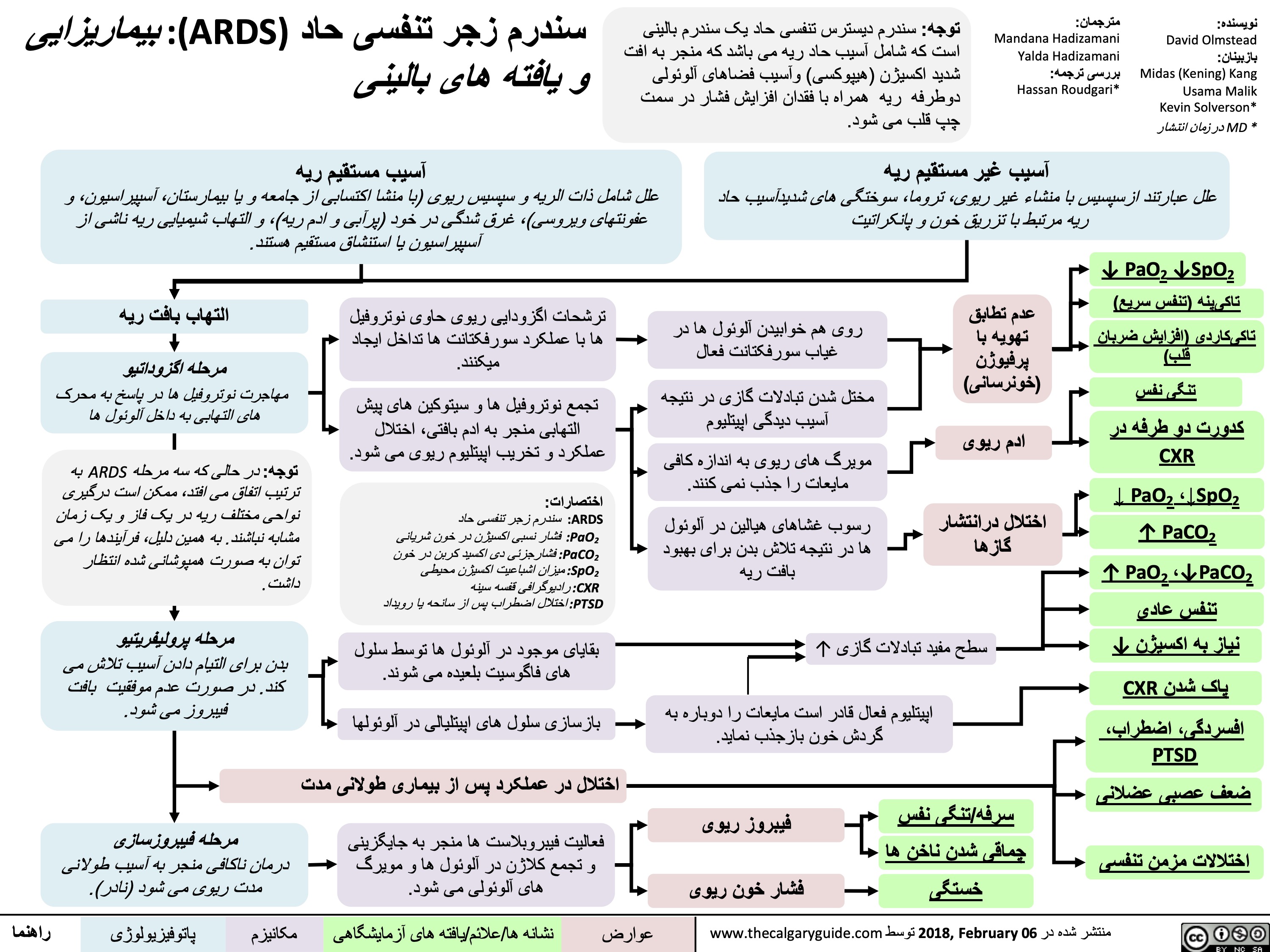
سندرم-زجر-تنفسی-حاد-ards
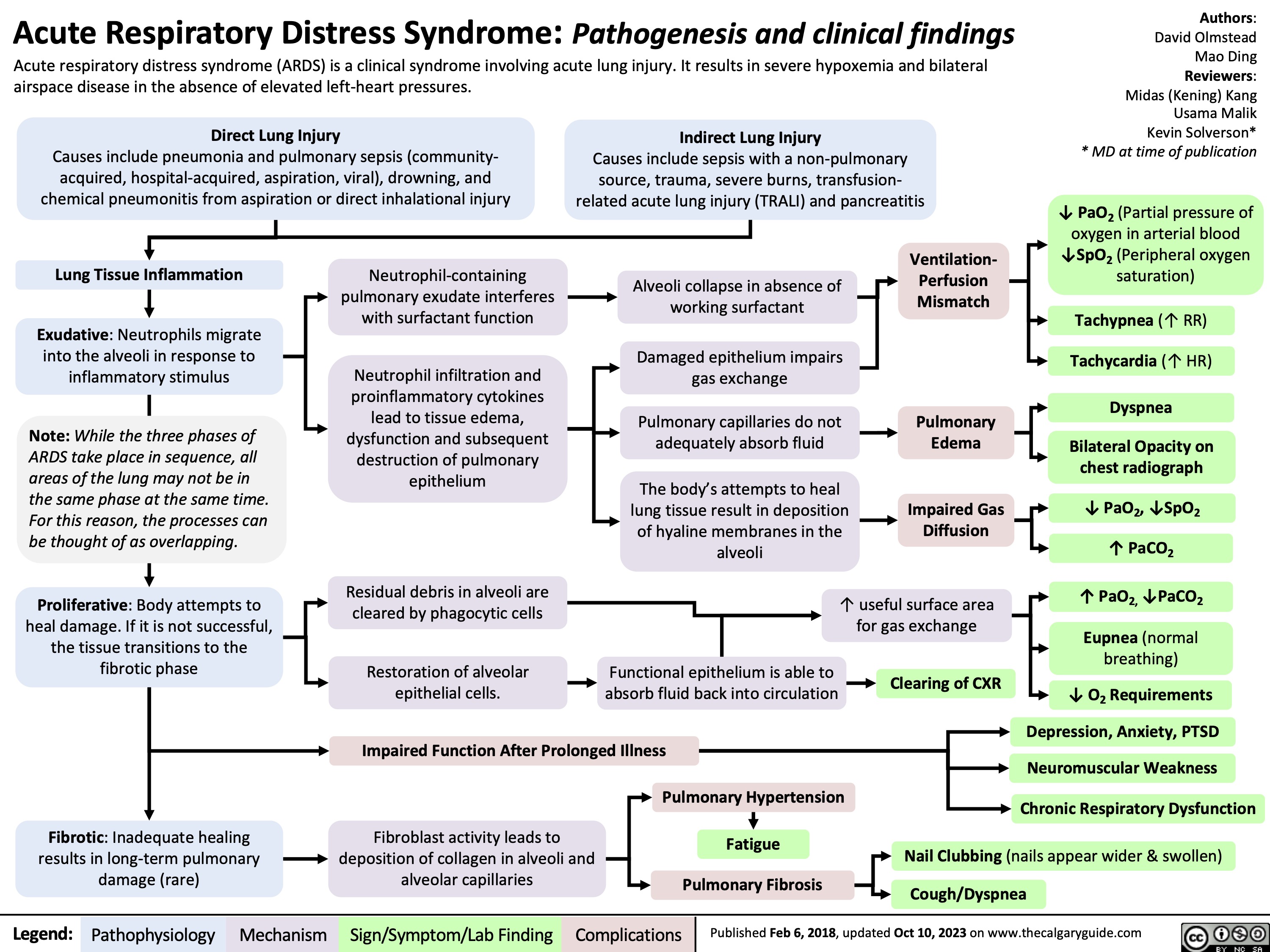
Acute Respiratory Distress Syndrome
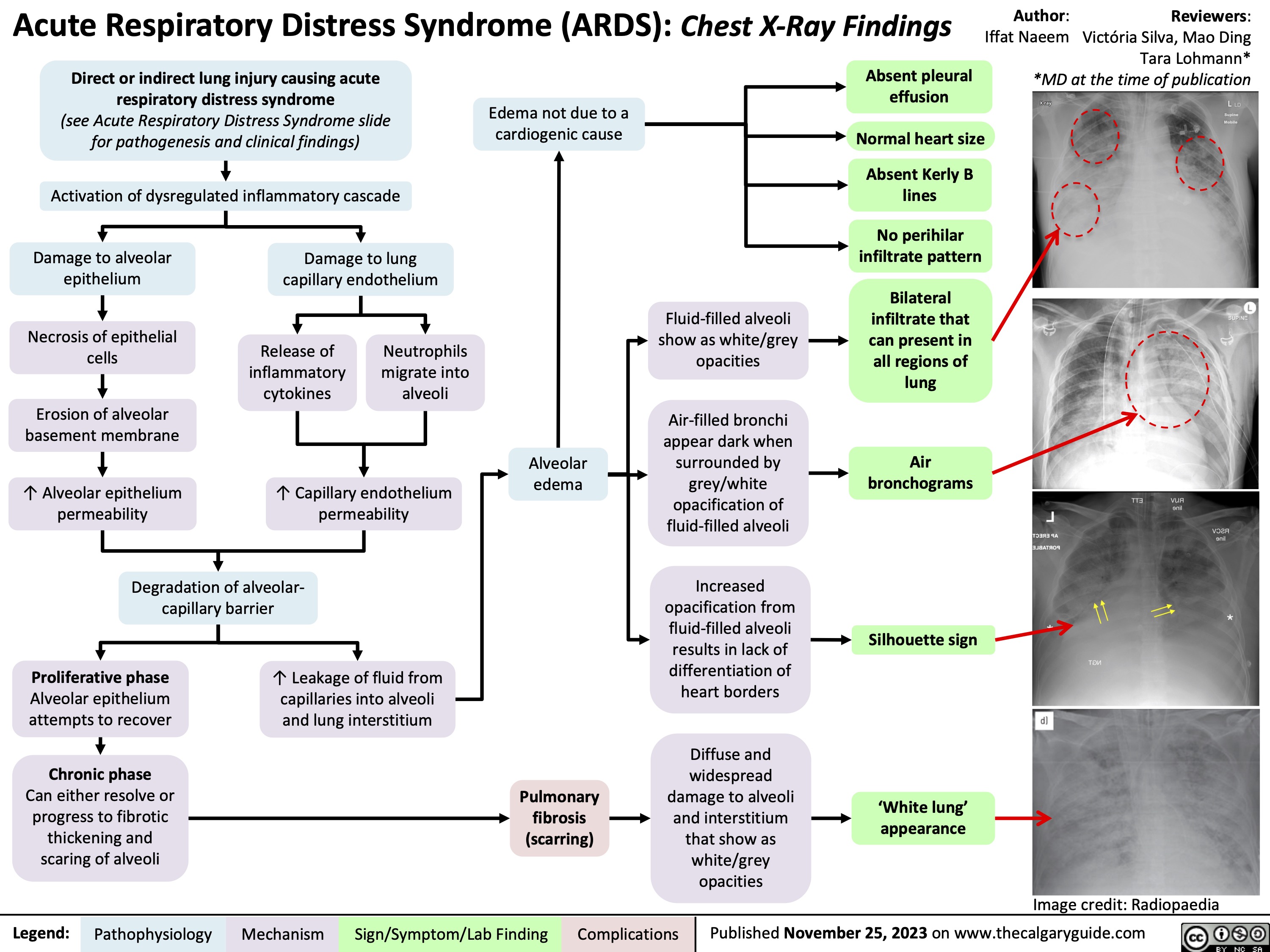
Acute Respiratory Distress Syndrome ARDS CXR findings