SEARCH RESULTS FOR: sickle
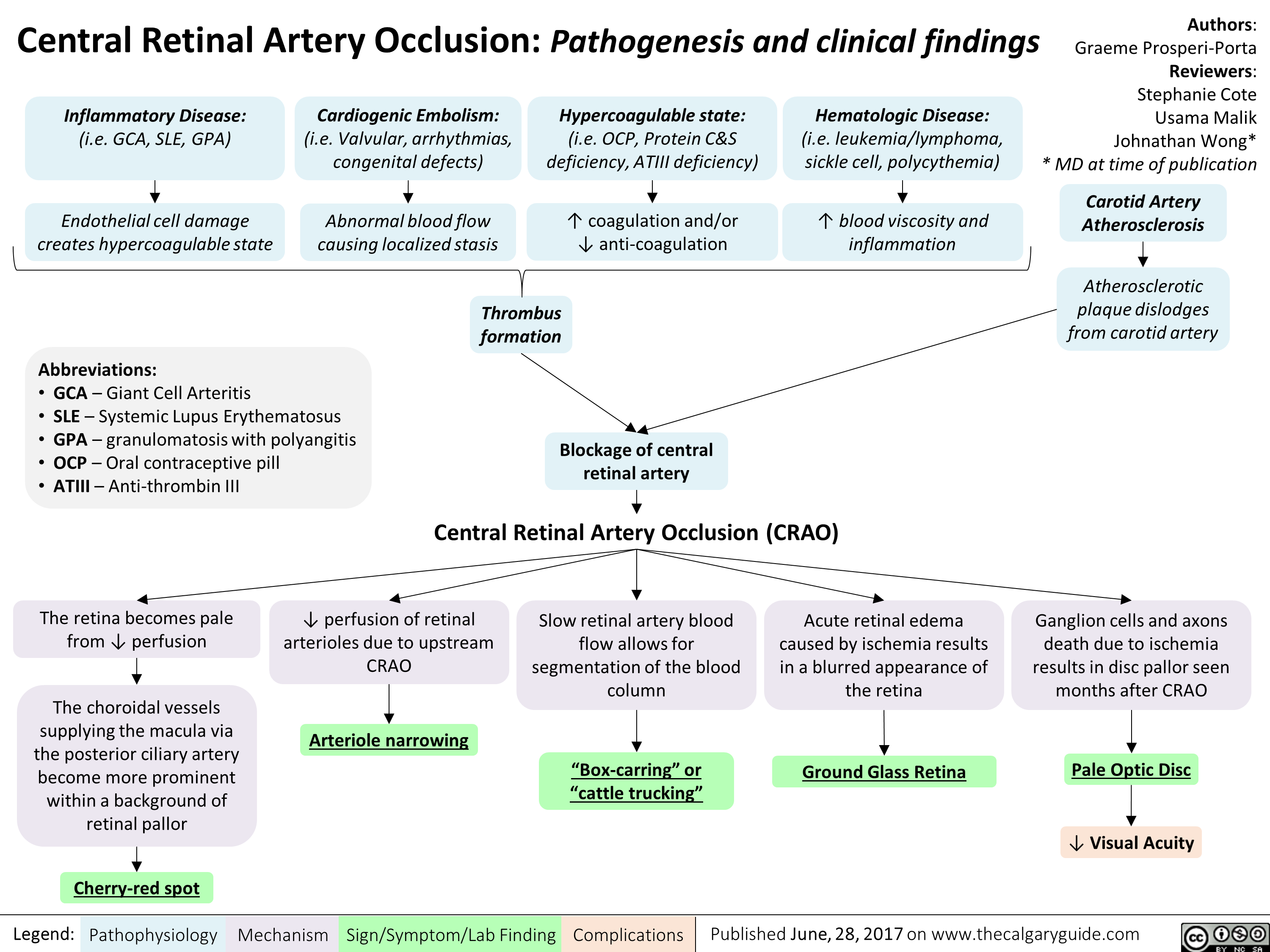
central-retinal-artery-occlusion-pathogenesis-and-clinical-findings
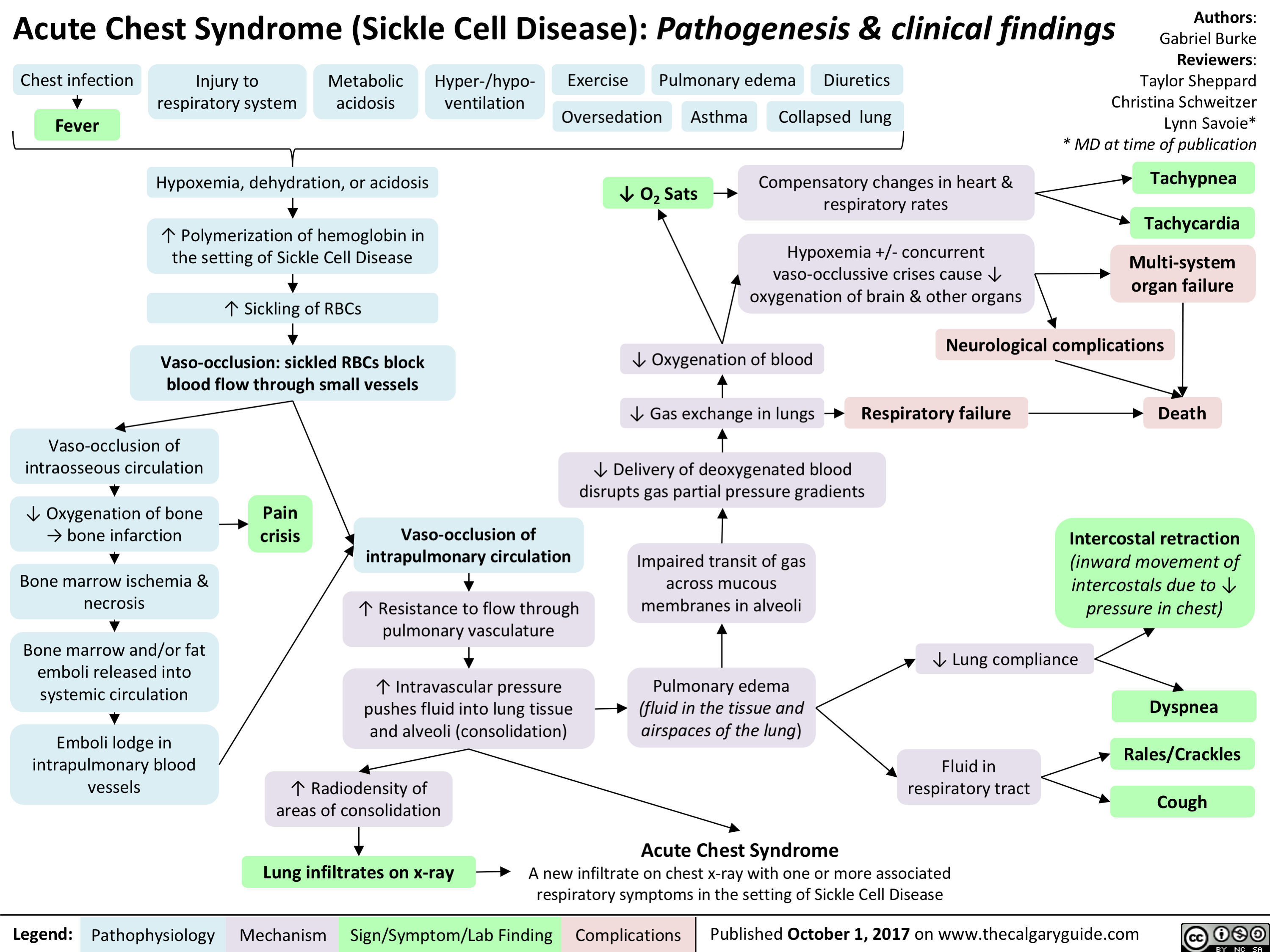
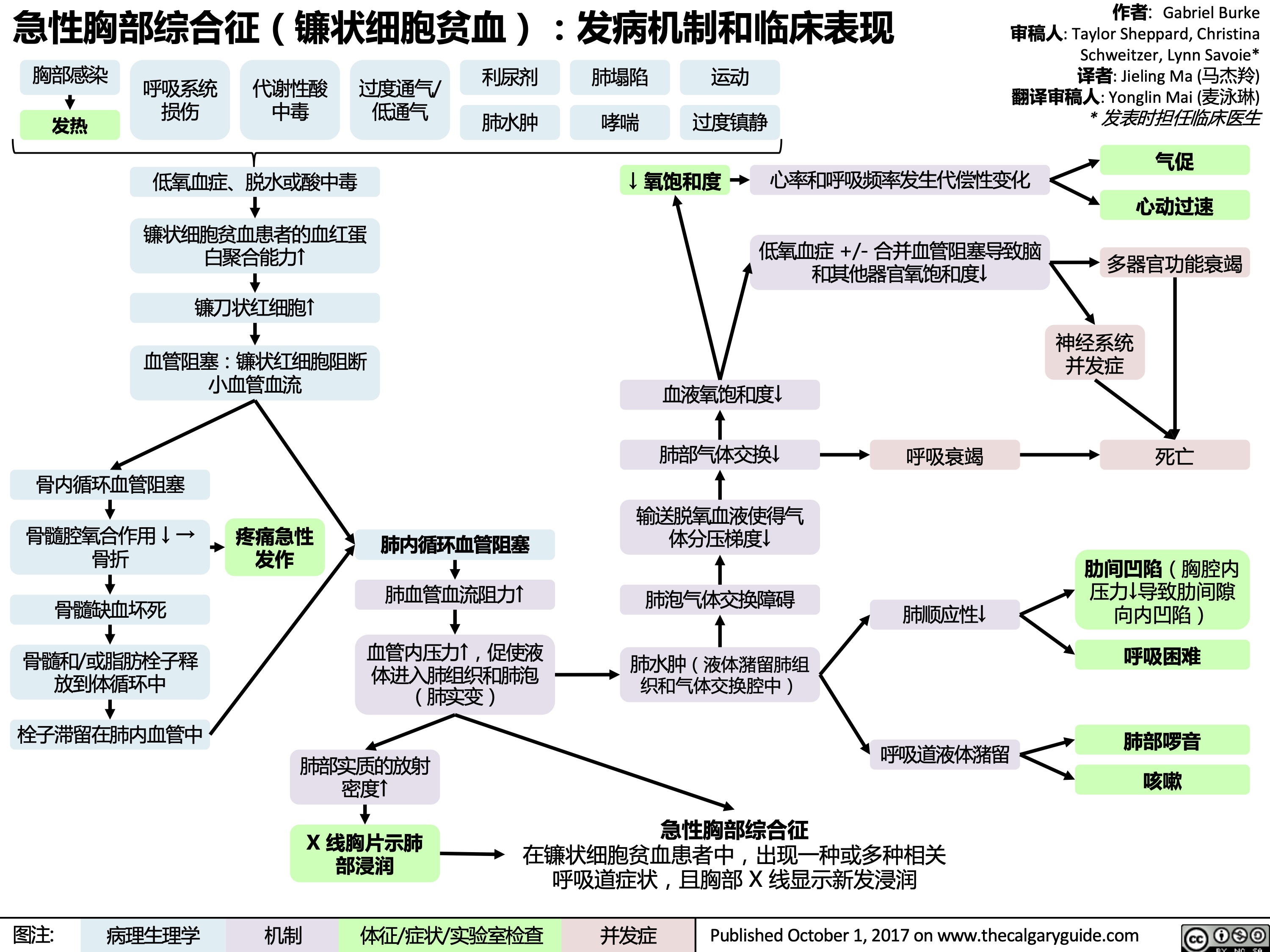
Acute Chest Syndrome (Sickle Cell Disease)
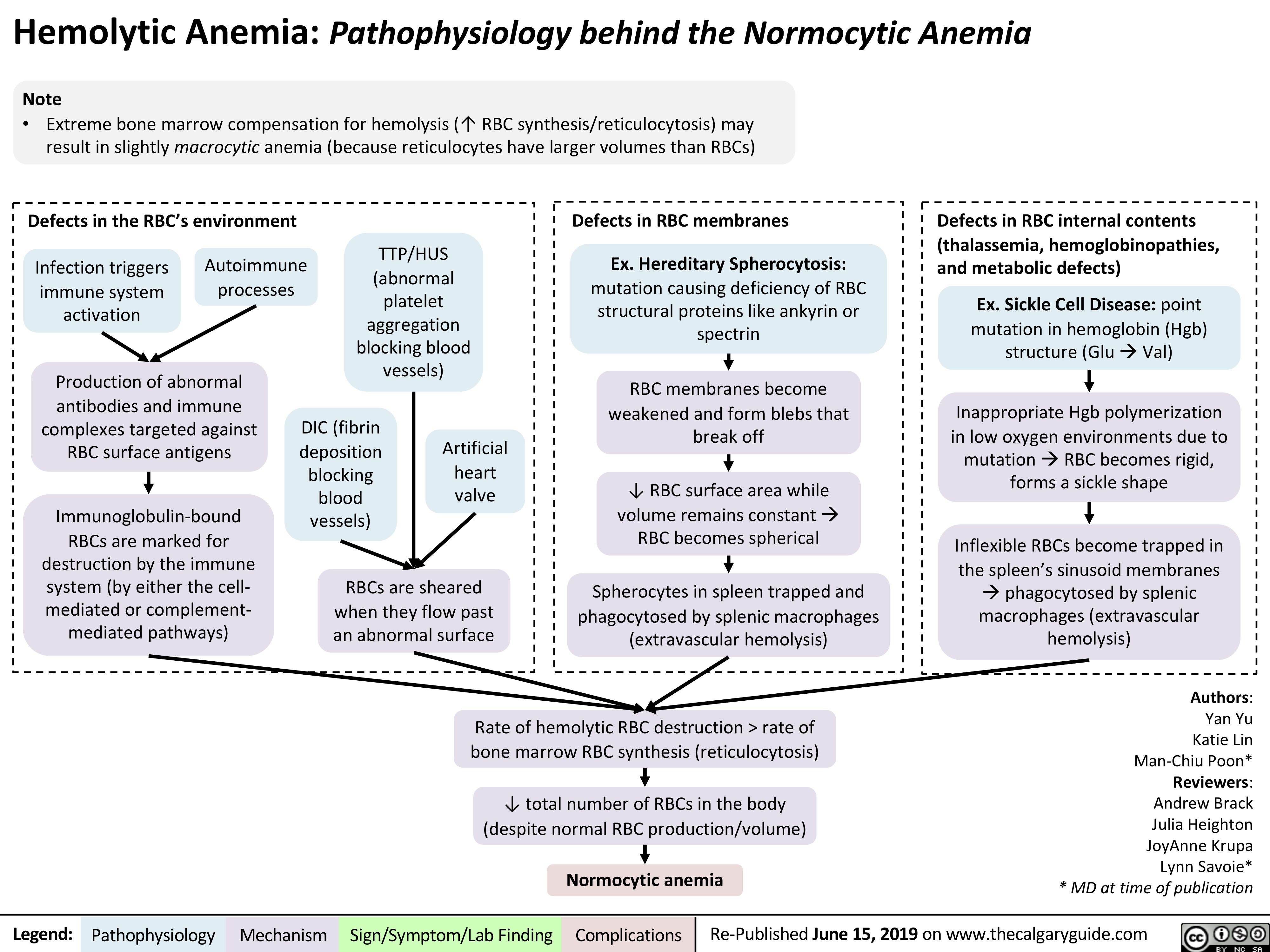
Hemolytic Anemia - Pathophysiology
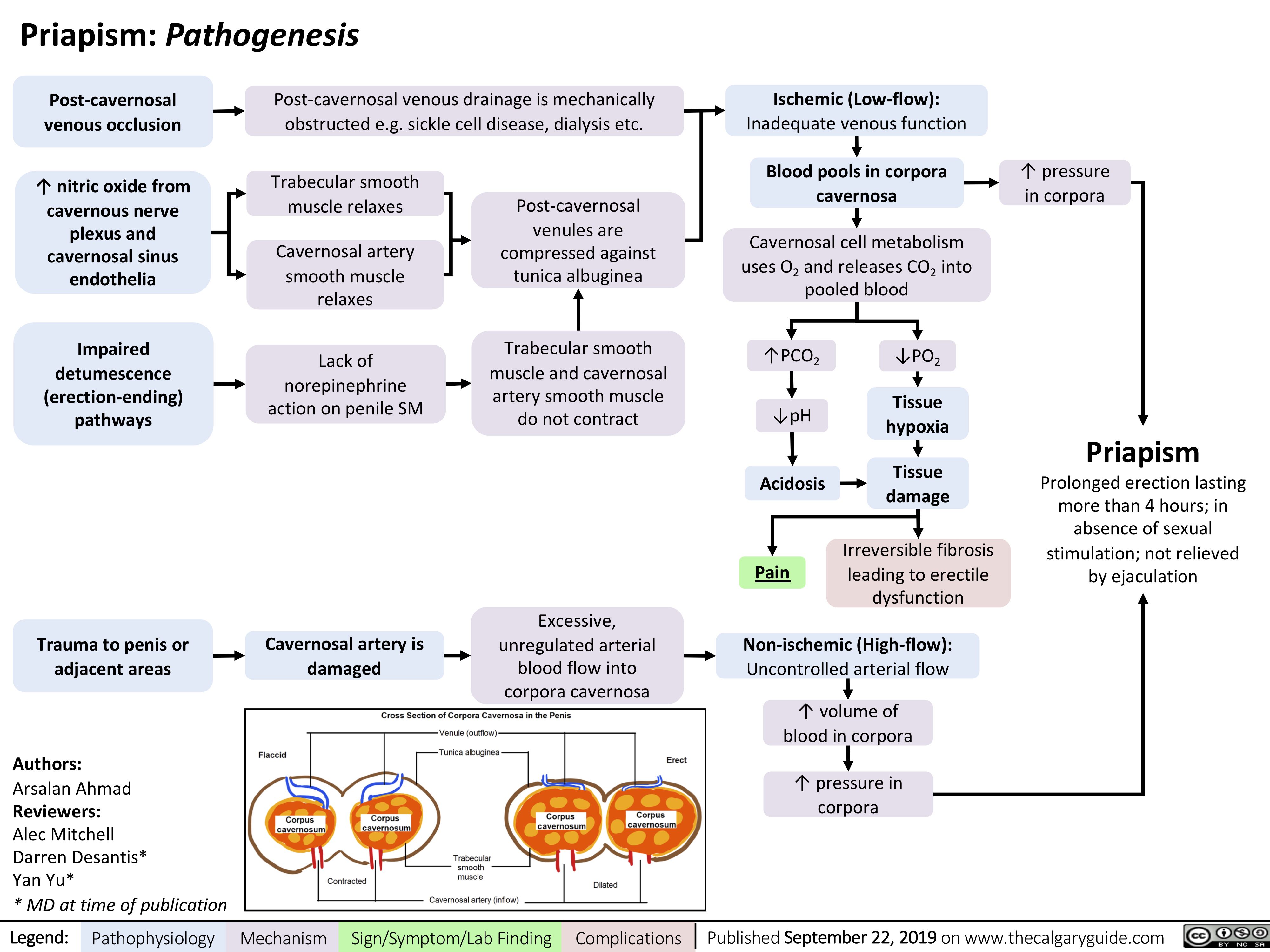
Priapism
急性胸部综合征镰状细胞贫血发病机制和临床表现
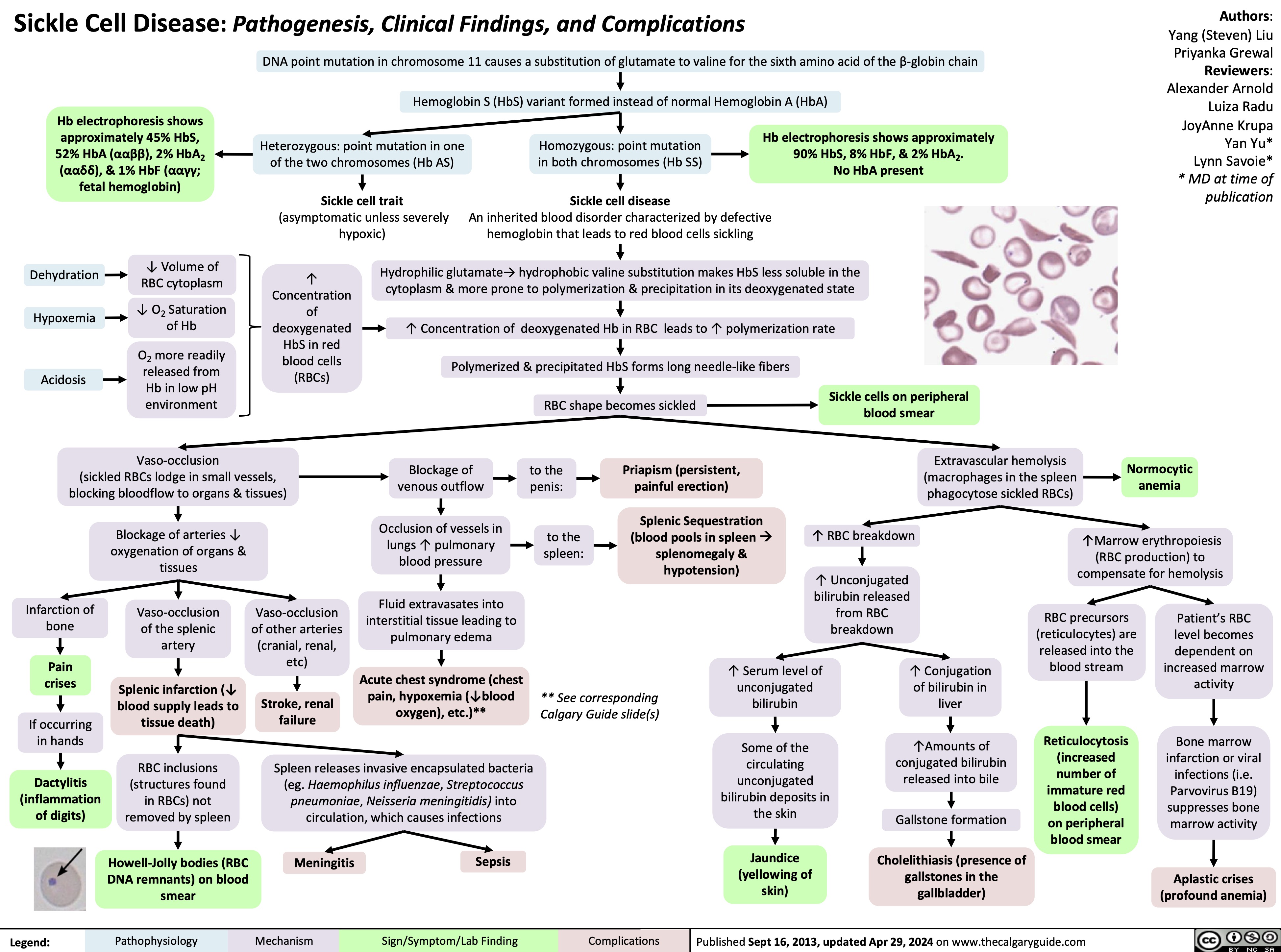
Sickle Cell Disease Pathogenesis Clinical Findings and Complications
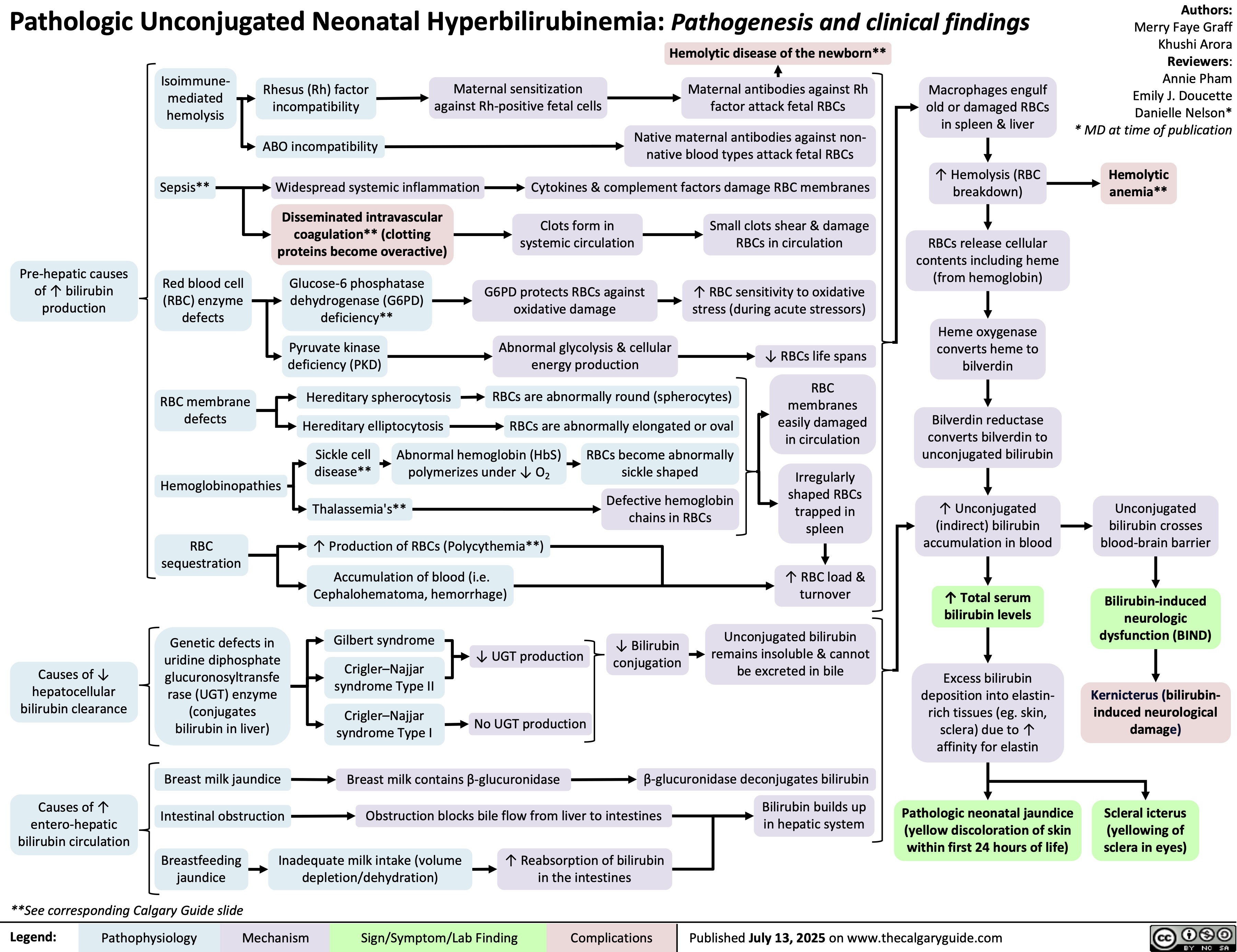
Unconjugated Hyperbilirubinemia